THE DEFINITIVE GUIDE: Calf Cramps & Other Calf Injuries Runners Encounter
You’re excited to see your best friends and debate your next race entry… you’ve wanted to do a destination Ragnar Trail but your opposition wants to train for the local half. Lame! You’re plan is to show them the online pictures…that’ll sell them!
The crisp autumn air hits you as you crack your car door. Summer is over, but this is the best time to run. It’s only cold during your warm up but it’s amazing after the first mile!
As you start hitting a quicker pace, the group’s conversation slows and becomes drowned out by the sound of running shoes hitting pavement. The challenge/ pain begins… this is why you’re here. This is when you feel the most alive and work on improving your race pace.
You tell yourself, “Focus… just focus on the logo on Joe’s shirt. He’s got a steady pace and always pulls you through. How the hell is he so strong at the end?! Just another ¼ at this pace and we are done…”
You feel great at the end… taxed but great. Now’s the time for breakfast and coffee!
That’s a great Saturday morning isn’t it?
What would you do with your Saturday? When would you see your friends?
This is a reality for people with calf cramps. Many of them cut milage from group days and don’t get to the push their pace. Luckily the injury doesn’t affect their ability to eat with everyone.
If you have a calf injury like this, it don’t have to be the end of your Saturday ritual.
In this guide, I’ll be going into the 14 things you need to know, change and try for calf cramps/ pain limiting you from a happy life.
I’m Dr. Sebastian Gonzales, from Huntington Beach CA, and I spent 18 hours of my life writing this guide for your injury recovery. Come see me if you’re in SoCal… if you’re not then I can direct you to a great doc.
Just contact me. Enjoy!

Chapter 1: Take walk breaks
Chapter 2: Break your workout into segments
Chapter 3: Slow your pace
Chapter 4: Warm up more completely
Chapter 5: Do you core work
Chapter 6: Add myofascial release at least once weekly
Chapter 7: Drink more water
Chapter 8: Test out electrolyte supplementation
Chapter 9: Improve your diet for two weeks
Chapter 10: Build your stretch shortening cycle
Chapter 11: Increase stiffness of the lower leg with exercise
Chapter 12: Take breaks as gait breaks down
Chapter 13: Run on softer surfaces
Chapter 14: Q & A about Calf Pain
Diagnosis 1: Muscle Tear (Soleus Strain)
Diagnosis 2: Achilles Tendonitis
Diagnosis 3: “Charley Horse” (Calf Cramps)
Diagnosis 4: Deep Vein Thrombosis (DVT)
Diagnosis 5: Baker’s Cyst
Diagnosis 6: Posterior Compartment Syndrome

Perhaps you might notice during hill workouts that your calves cramp more?
This would be an example of your neuromuscular system not being ready for the load of the hill. Adding in threshold training to prevent calf cramps can greatly improve both your race times and your comfort level.
If you haven’t done this before, you’ll be surprised about how challenging it still is.
Think of this as more of a temporary compromise. When calf cramps are due to jumps in your training volume, the muscle and tissue within the calf is telling you it’s not ready for the increase in mileage. A decreased pace can improve your ability to withstand jumps in volume while minimizing your risk of chronic calf cramps.

Other goals in a warm-up will depend upon a runner’s individual needs. Some runners need more trunk stabilization, others need more hip mobility, and some of them need thoracic spine mobility. If it were up to me, no two runners would warm-up the exact same way.
When I say you need to have a more complete warm-up, I mean one that enables your body to perform better as a unit. You can go back to what I said just a few lines ago: if you have poor trunk stabilization, you have a high probability of hip drop, which leads to more lower leg injuries and calf cramps.

No body motion, including something as complex a running gait, is possible without a functional core. If you want to read about the way the core works, go to this page of my site. Yes, it is page on low back pain, but I promise that it correlates to calf pain.
It will have everything you need on this topic.

When we consistently loosen the calf muscles, we also decrease our potential to spring off the ground. Using a skilled manual therapist to find focal locations of adhesions is the best way to add soft tissue work/myofascial release into your weekly routine.
Can you do it on your own? Sure, but clinically, we often see that there is a minimal effective dose. Too much is bad for your gait, and too much in the wrong spot is also bad for you. So, yes, you can attempt on your own, but doing so could make you slower and more injury prone.
Some of you are probably thinking, “But it feels good!” Ya, it does–trust me, I get it. But alcoholic beverages “feel good” too, but if drank in excess or without eating, then I’m sure you won’t be feeling good for long. I think we can do it selectively.
There are other ways we can increase our range of motion at the hips which will save the calfs. Listen to this podcast for more on this.
If you weight is 130 pounds, divide it by 2.2 to see your body weight in kilograms. In this case, it’s 59 kilograms.
So, this “inactive” person needs to drink 59 ounces of water a day. That’s 7.3 cups. If you’re training hard, I would shoot to double that.
Here’s a cool water calculator you can use.
I can’t tell you how many triathletes I saw sidelined at Wildflower when the temperature hit the high 90’s during the run. I had some extra salt supplementation, so I gave it to one lady. She was up and moving again within 20 minutes. The cramping can be so severe, it can DNF you.
What are some electrolyte options?
Salt stick is the only product I’ve used. It is killer.
- Eat eight different veggies a day (credit Dan John)
- Greener and leafier the better
- Eat healthy, unbleached complex carbohydrates ( Ie: Sweet Potatoes, Oatmeal, Brown Rice etc.)
- Don’t overdo the fruits
- The lower the glycemic index the better
- Get your protein ( 1.7g per kg body weight)
- No more than 30g per meal (female) and 40g (male)
- Drink your water
- No fast food, refined sugars, or processed food
Charles Poliquin has a great write up on some better choices.
Here’s why:
The stretch shortening cycle is where the elastic properties of the muscle/tendon complex (in this case, the calf region) builds up energy from landing and assists us with our next step. It’s like free energy!
Another example is a hybrid car: they gather energy from their brakes when they stop and reuse it as electricity. Genius right? The body is smart like that too, but we have to train it to optimize this energy-saving mechanism.
To learn more about how to train the stretch shortening cycle, check out my comprehensive article here.
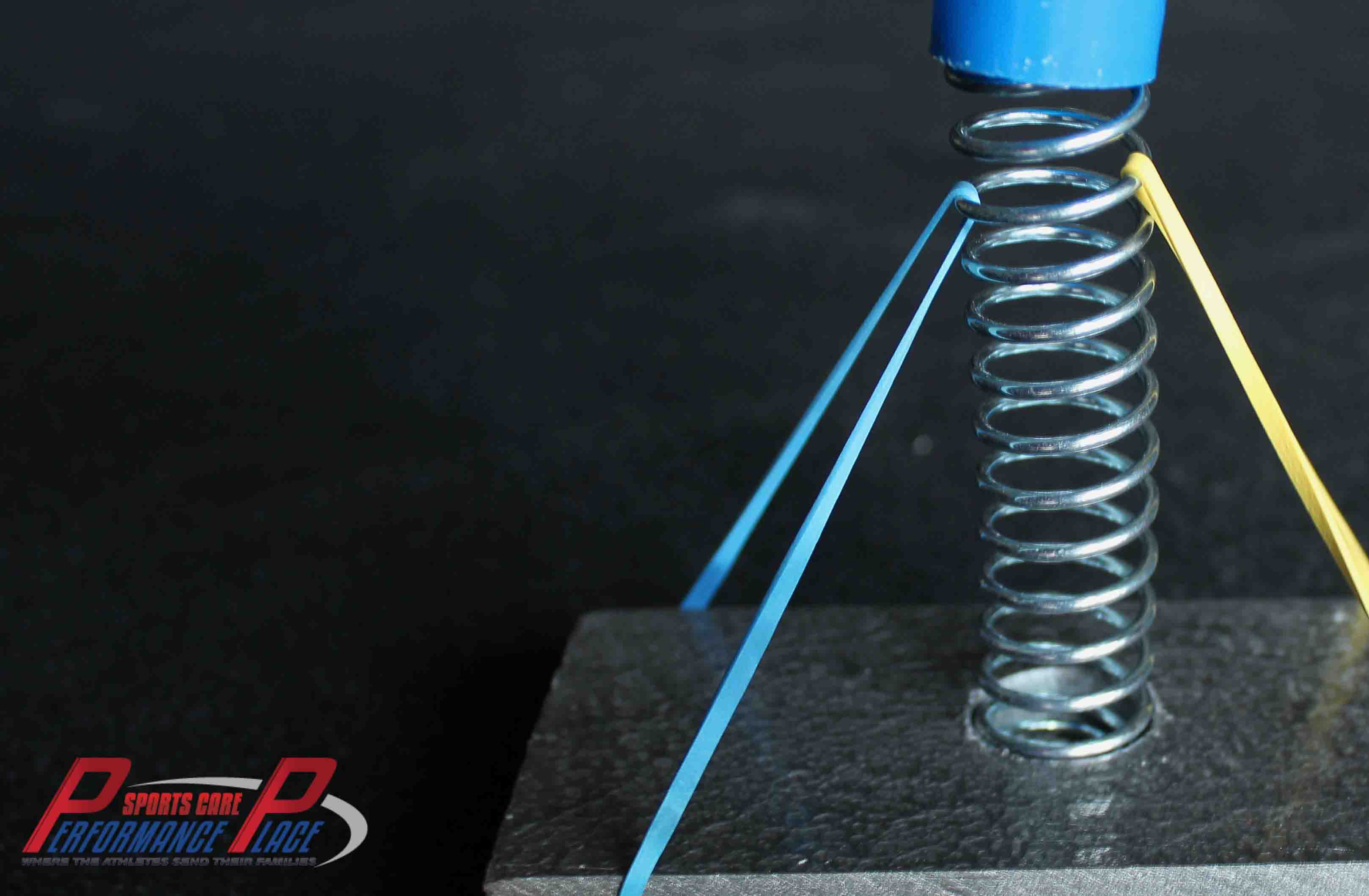
That is one of the best ways to improve lower leg stiffness, but constant stretching, foam rolling and tissue work decreases the rubber band’s ability to transfer energy, like the hybrid car does.
If you take proper breaks, you will spend more time running in good form rather than training in “compensation mode” for the majority of your miles.
If you don’t understand this concept, listen to the podcast… it will blow your mind!
This will not correct your gait issues, but it will keep you sane as we are adjusting other parts of your body that are lacking (core endurance, hip range of motion, functional capacity, etc).

What Causes Soleus Muscle Pain?
Soleus pain often feel like a deep soreness in the lateral (outer) aspect of the calf. The soleus muscles can become strained with running, speed walking, and jogging. Typical mechanism of injury is overuse (no trauma). It is treatable with time of recovery ranging from weeks to months. Soleus and gastrocnemius muscle pain can be found together.
Why do my calves hurt while running?
There’s many different reasons why your calves can become painful or even cramp while running, but one of the highest probable causes is poor running gait. I have a friend that I casually run with who often develops calf cramps after just a few miles. Watching him run, you can clearly see his excessive vertical displacement… it’s like he’s bouncing up and down rather than running forward.
Through my clinical experience, I’ve found that runners with poor core endurance and poor hip extension will often report more calf pain, calf cramps and ankle “overuse” injuries.
How can you improve your core?
The concept of core training have changed a ton over the years. Here’s a few of my favorite exercises:
- McGill Curl Ups
- Side Bridge
- Birddog
- Suitcase Carries
These are called isometric core exercises, and in my opinion, they are the very best at improving your midline stabilization. Some examples of non-isometric core exercises are Superman Pumps, Russian Twists, and Standard Sit-ups. I suggest people start with four times per week for about 20 minutes. I plan to have an entire page on core exercises. When it’s live, it will be HERE.

Here’s the simple answer: the entire lower limb works as one unit, and if we want to be specific, it can’t properly function separately from a properly functioning hip, core, and nervous system. A properly functioning core (midline stabilization) is what allows our hips to move us powerfully forward in our gait cycle. The core allows for stabilization of the hamstrings and quad group to work and decreases the “overuse” of the calf group. Let’s not blame the squeaky wheel here!
Why do my calves hurt? What’s the Diagnosis?
These are the top diagnoses we see in the calf in the endurance athlete population:
- Muscle Tear (Soleus Strain)
- Achilles Tendonitis
- “Charley Horse” (Calf Cramps)
- Deep Vein Thrombosis (DVT)
- Baker’s Cyst
- Posterior Compartment Syndrome

How long does it take to recover from calf cramps?
Calf cramps typically self-resolve, however you can accelerate the recovery time by gently rubbing and relaxing the muscle quicker. The longer time it is spent in contraction the longer the recovery time.
A stretch that can be done almost anywhere is a wall stretch. (PIC TO COME) You put your heel against the ground and toes up on the wall. Gently lean into the stretch just to elongate the muscle. This is definitely not a stretch you want to to do aggressively because you risk increasing cramps with aggressive stretching as well.
The application of heat (shower or compression wrap) to the calf can also decrease cramping. It’s important to note that if your calf cramp is from a DVT (deep vein thrombosis) this can actually make it worse–and kill you, seriously.
Anytime I hear of someone with calf cramps, especially if they’ve been traveling or had past, recent trauma, I strongly suggest they go to their doctor/ER to confirm they don’t have a blood clot in the vein of the calf.
How do you stop getting cramps?
- Train appropriately
- Drink enough water
- Account for temperatures when training
- Make sure your body has adequate salts
- Eat well
Notice majority of my suggestions are based upon things that you can change. I’ve met many people who have said they have chronic calf cramps and (lo and behold!) you find they are eating poorly and poorly programming their training sessions. Calf cramps are completely preventable if we treat our body like a temple, stop destroying it and putting bad things into it.
My current opinion on how to prevent cramps has changed over the years as studies have lead me away from the electrolytes and water issue. I’ve found “less than great” science shows that cramping has anything to do with electrolytes and water and more evidence to show calf/ankle and foot issues in runners comes from core endurance (ie: hip drop), neuromuscular degrade (form breakdown) and conditioning.
If you want more info on how running injuries occur from neuromuscular breakdown, you should read the chapter in my huge article on running tips HERE.
DIAGNOSIS 1:
CALF MUSLCE TEAR
Type 1 – minor strain/tear (no bruising)
Type 2 – moderate tear (bruising)
Type 3 – complete tear (bruising and deformity)
Currently, we do have a more elaborate grading system for muscle injuries, which was developed in 2012. I have a whole podcast on this one topic, but here’s a little article you can read along with it as well.

- Extremely tight calf muscle?
- Have to stop running to stretch?
- Rolling out constantly with no improvement?
- Calf muscle pain after running?
- Calf tightness while running?
Speak to someone at: Support Center here.
Calf pain while running can be extremely frustrating.
With proper rehab and treatment, you too can overcome these injuries…BUT you have to make sure that you first have a correct diagnosis.
SOLEUS STRAIN
- Dull, throbbing ache in the middle of your calf?
- Deep cramp in the lower leg?
- Have to halt your run and hobble back to the car?
- Pain walking down stairs?
- Calf pain while running?
These are how some of my runners have described their soleus strains. These are not the only symptoms of a soleus injury, but they are typically the most common complaints.
You do not have to continue suffering from a calf injury. If you have been diagnosed with a soleus muscle strain, this article will greatly assist you in understanding your rehab.
You are probably wondering, “Should I run with calf pain?”
I had a conversation like this with a running coach at my office just yesterday about this.
He wanted to just “go test” it.
So, I asked him candidly…
“Have you done all you can to responsibly rehab it?”
Without going into his answer, if your answer is “No”, then I would tell you not run with calf pain.
What is a Soleus Strain?
A strain is a small muscle tear. They are typically called “micro-tears”. By clinical definition, they are also called Grade I soleus muscle tears.
Wondering if you have a Grade II tear?
Grade II tears will normally have some visible skin bruising due to a greater degree of muscle tearing than a Grade I.
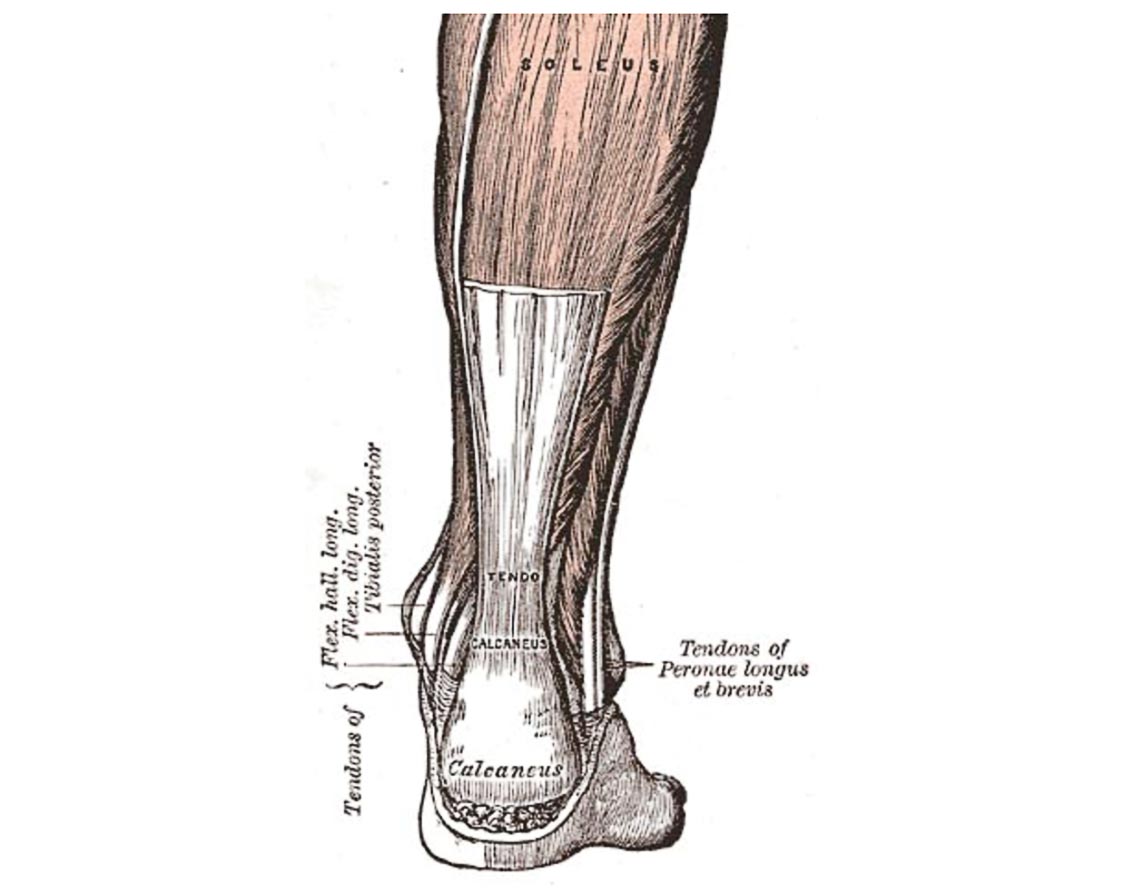
The soleus muscle is one of the larger muscles of the calf, which attaches to the heel via the Achilles tendon. The soleus actually makes up the majority of the calf muscle if we were to assess it by volume.
The soleus muscle is considered a slow twitch muscle and for that reason, it carries you through a run. Its internal composition allows it to produce more endurance than the overlying calf muscle, the gastrocnemius.
What Causes a Soleus Strain?
Soleus strains happen for many reasons:
- Overtraining
- Poor fitting shoes
- Hill training
- Over pronation/flat feet
- Poor core strength/endurance
- Poor hip flexibility
- Poor hip strength/endurance
- Gait abnormalities
You see, there are several potential underlying causes.
The reason for your injury would have to be tested.
I call it the “white elephant” in the room.
Do you visibly have flat feet? No…let’s move on.
Are you more flexible than most of your friends? Yes…let’s keep looking.
Do you do core training for 15 minutes or more three times a week? No…ok, now we are onto something!
I would test your core and hips to see if there is below average strength and/or endurance, and if there was, then gait breakdown under strain is your most likely culprit.
The “white elephant” is the top target on the rehab hit list, and it’s usually the thing you smile and say “Noooooo” to when asked if you do it or not.
How can you Rehab Calf Pain while Running from a Soleus Strain?
Let’s say we keep going on the same track: your feet looked good, your flexibility looked better than average, and your core strength was suspect.
I’d test your core in three planes of motion:
- Forward and backward
- Side to side
- Rotate and rotate
That is six motions total in three different planes.
Perhaps we’d find that your rotation stabilization was poor and your extension was too.
I’d suggest you do the Birddog exercise because it challenges those two motions.
If you failed in flexion and rotation, I may give a Dead Bug exercise.
Here’s a video of a good friend of mine doing these two exercise progressions:
Of course, there is a lot more to rehab than just these two progressions, and we have an advanced online course we will be offering.
If it is up, you will see a link HERE.. if not, then it is coming, I promise.
What Kinds of Treatments can be done for Calf Pain while Running because of the Soleus?
For decreasing pain associated with a soleus strain, I really like these treatment options. They are extremely effective, but even though your pain decreases, you’ll still need to rehab the “white elephant”.
- Joint Mobilization
- Immobilization
- Soft Tissue Mobilization
- Eccentric Exercise
- Postural Endurance
- Dynamic Mobility
- Nutritional Changes
- General Strength
- Plyometrics
- Movement Pattern Correction
- Co-contraction
- Appropriate selection of milage
- Appropriate selection of intensity
- Surface Consideration
- Footwear
- Athlete Goal Setting
- Co-management with coach, strength coach, etc.
Here’s a self-muscle release video you may be interested in:

- Muscular fatigue (lots of miles or low mileage with poor form)
- Dehydration
- Electrolyte imbalance
- Poor diet
- Various systemic reasons
One of the best recommendations I can give you for calf cramps is to look at your diet and water intake. If you’re not eating and drinking water like an athlete, you don’t deserve to be an athlete.
A deep vein thrombosis is a blood clot in the deep vein of the calf. When massaged, this blood clot can dislodge and move its way to the lungs which often results in death. Typically, a DVT will have a stereotypical history, but there have been cases that are far from textbook. If we suspect a DVT, you must go to the ER now.
Common history findings with deep vein thrombosis are:
- Recent surgeries
- Long plane flights
- Sitting for long periods of time
- Genetic predisposition/family history
However, it’s important to remember that even if you don’t have these common textbook precursors, it is still possible to have a deep vein thrombosis. I strongly urge you to visit your nearest emergency room, especially if you’re having difficulty breathing.
Can you stretch it?
No, because it’s not an injury to a muscle or tendon. Oftentimes, knee injuries are highly correlated with dysfunction or lack of proper use of the ankle or foot, the hips, and/or the core.
- Lower leg pain that begins during exercise (not before)?
- Lingers for about five minutes after stopping?
- Feels like pressure in the calf?
- Foot tingling?
- Calf pain while running?
These are all symptoms of Posterior Compartment Syndrome of the leg.
As we go through this article, I am moving through the conditions from those that I would prefer you have to the ones that I’d rather you not.
Posterior Compartment Syndrome is much harder to treat. I have had some runners who’ve had to actually change sports because of its re-injury rate.
I have compiled the information I think you need to know about this painful calf condition. Beyond this information, you may need to speak with someone in person.
Do not try to tackle Posterior Compartment Syndrome alone. It is so much more complex than normal calf pain while running that most of you experience.
What is Posterior Compartment Syndrome?
Posterior Compartment Syndrome of the leg is a compression condition. Compression occurs in the deep, backside compartment of the leg from swelling. Excessive compression of the blood vessels and nerves in the area ultimately forces you to stop moving. Lack of blood supply means less oxygen for your muscles. Nerve compression means tingling and altered function of the muscles they control.
This is boring stuff, right?
Hang in there, the rehab section is much more fun.
What causes Posterior Compartment Syndrome?
The compression of the vessels and nerves is what causes the pain and swelling. The compression can come from structures that are within the compartment being too large. We believe the muscle grows too large and decreases the free space for everything else.
Some feel the muscles increase in size due to excessive demand or workload, such as with flat feet or poor footwear. I feel improving gait patterns is a better answer, since ground contact force will increase with gait abnormalities as well. Correction of the foot and ankle is only half of the battle.

How can you rehab Posterior Compartment Syndrome?
So, is the answer to decrease the size of the muscle?
In theory, rest would do that, but no, that is not the answer. Rest will assist in keeping the symptoms at bay, but it does not improve gait, striking patterns, core strength, ankle/foot strength and more. We need to decrease the workload put on the muscles of the deep compartment.
How do we do this?
Improve the function of the entire kinetics chain (core, hip, knee, ankle, foot etc.) I like to start at the core and hip.
Here’s a few exercises that I use with high frequency when I am working with a runner with calf pain.
The Lewit:
The Barbell Hip Thruster:
The Superman:
What kinds of treatments can be done for Posterior Compartment Syndrome?
There are several treatments that I attempt before getting too extreme on a surgical treatment plan.
Here’s what I normally suggest:
- Joint Mobilization
- Immobilization
- Soft Tissue Mobilization
- Eccentric Exercise
- Postural Endurance
- Dynamic Mobility
- Nutritional Changes
- General Strength
- Plyometrics
- Movement Pattern Correction
- Co-contraction
- Appropriate selection of milage
- Appropriate selection of intensity
- Surface Consideration
- Footwear
- Athlete Goal Setting
- Co-management with coach, strength coach, etc.
Here’s a self-muscle release video you may be interested in: