- Lumbar Disc Herniations
- Pinched Nerve In Lower Back
- Arthritis
- Low Back Muscle Strain
- Sciatica
- Spinal Stenosis
- Trigger Points
- Facet Syndrome
- QL (Quadratus Lumborum) Spasm
- Weak Multifidus Muscle
- Being out of alignment
These are the most commonly talked about reasons for lower back pain. If you feel like one of these is your reason, you’re in the right place. This article will debunk many myths surrounding back pain, based upon current research.
You’ve been suffering from on-going lower back pain you probably have not found the right solution yet. The majority of people can return to a pain-free life and full activity after a span of lower back pain IF you use the correct type of treatment for your problem.
In this article, we will unravel some of the inefficient care you may have been trying with little results.
Your body is resilient and can get better. Lower back pain was once thought of as diseases that create irreversible damage in the spine. The current thought is that back pain is more like the flu. It is a temporary issue and will not have long-lasting negative repercussions on your life. Yet much like having the flu for years on end, you may suffer from undesired body compensations.
I have had lower back pain twice in my life, once at 16 and again at 38. I have a 2 mm central disc protrusion. I have had leg pain, back stiffness, the inability to bend forward or tie my shoes. I have been where you are. Allow me to show you what I have learned through both of my recoveries.
The first year I was in pain, I lost an entire high school baseball season. I tried PT, meds, rest, imaging, chiropractic, acupuncture, reflexology, Active Release, physiotherapy, strength training, massage, and much more.
Looking back, I saw how much time I wasted and continue to waste today when I encounter a new injury and default back to what I “thought I knew.”
I followed what my parents and friends told me:
- Ice
- Heat
- Rest
- Stretch
- Surgical consultations
- Consideration of dropping my sport
Many peers told me I would have a “bad back” for the rest of my life.
They were wrong, and after becoming the director of care at a sports injury clinic, I now know that 90% of what they’d advised me to do was wrong.
I encounter back pain patients every day and see they are where I was back at 16; hence this article.
My intent for this article is to stop you from doing things that will hinder your spine’s ability to heal. Your spine wants to improve. You just need to allow it but not picking the scab.
At the end of the article, I’ll cover the 5 Steps of Lower Back Recovery. Check the sidebar if you’d like to jump ahead.
After finishing this article, you will know all of the current TRUTHS about back pain therapy and treatment. We will start by discrediting the most common “truths” that you have probably heard.
Therefore, I am calling this article: THE 12 MYTHS OF BACK PAIN
Note: I’ll give you a hint, most unsolved lower back pain is from a low back disc injury, which can be corrected without medication, injections or surgery. Contact us if you want a real game plan for getting better.
THE “RED FLAGS” OF BACK PAIN
Before we start, you should know we group back pain into three categories:
- Category 1: Non-specific low back pain
- Category 2: Back pain associated with radiculopathy or spinal stenosis
- Category 3: Back pain associated with another specific cause
Your category dictates your treatment plan.
For Category 1 and 2, we usually recommend going with conservative care for a month or so and see if there is improvement.
With Category 1, we have an extremely high success rate.
With Category 2, we have a little less depending on the severity of some of the underlying issues.
With Category 3, we usually refer out to a specialist. Your back pain could come from other odd conditions such as infection, cancer, referred pain from other organs such as gallstones, and more. A doctor in another specialty can assist in these cases.

The “red flags” of low back pain are the only reasons we should attribute pain to a structural cause.
The “red flags” are:
- Progressive motor or sensory loss
- Bilateral leg weakness or sciatica
- Unexplained weight loss
- No improvement with 6-8 weeks of conservative therapy
- History of trauma
- Saddle anesthesia
- Urinary or fecal retention
Now that we have all of our categories and “red flags” out of the way, let’s get into the 12 Myths of Back Pain Article
Other Important section (click links to read immediately):
MYTH 1: REST HELPS
MYTH 1: REST IS THE KEY TO RECOVERING FROM BACK PAIN
Excessive rest is worse for most lower back pain. True story! (How I Met Your Mother reference)
Don’t believe me?
Reliable evidence shows those with acute low back pain who choose to follow advice for bed rest have more pain and less optimal recovery than those who stay active as the area heals (Hagen et al, 2005).
In regards to sciatica (leg pain with back pain), resting still doesn’t provide an advantage either. Your logical mind may be thinking, “If I rest, my back will get better.”
I don’t blame you for thinking that way. Let think of back injuries like ankle sprains, which are obviously different, but their recovery process has similarities. Acute injuries of the ankle, yield a typical and expected limp. The purpose of a limp is to remove weight from the ankle as regains the ability to tolerate full body weight. Time spent with a limp can between 5-10 days.
We can now grade the limp, from full limps to the barley noticeable ones. Recovery from an acute lower back injury is the same. Being on the ground for a day or two happens, it’s expected, but you should be spending less and less time on the ground over those 5-10 days. Most people I work with should be walking with no pain within a week.
But what about “non-acute ankle sprains.” Should we force a limp to occur? With minor back tweaks, should we force the bed rest?
In these situations, movement can be used as medicine. Coach was right, “walk it off.”
Back pain can produce an endless cycle if you let it. The muscles of the trunk (the core muscles, diaphragm, pelvic floor, glutes, and lats) are all skeletal muscles and will weaken with rest. Muscles weaken at a rate of four times faster than you can build them.
When the muscles become weak, then your spine takes more load, which can create more pain if your spine was unprepared for the load due to bed rest in the first place. The logical answer would be to keep the muscles of the trunk from weakening, right?
How can you do this?
Train the trunk to co-contract and train the ability to hold intra-abdominal pressure, which are both supportive to the spine (we will go into this later as well). Even if you don’t know how to do that, the above study shows that you will improve if you simply just get up and walk.
So why not stay active and enjoy life?
The evidence says you should.

Here are some easy, actionable tips I give my patients. I call it the 10, 20, 30 Rule:
- Get up and go for a 10-minute walk two times a day
- Get in and out of a dining room chair 20 times a day (use your hips)
- Practice getting in and out of bed/off the couch 30 times a day
Other Important section (click links to read immediately):
MYTH 2: STRETCHING HELPS
MYTH 2: BACK TIGHTNESS SHOULD ALWAYS BE STRETCHED
If you feel like stretching is the way to go, you are not alone. I would venture to say a vast majority of the U.S. population feels this way and rightly so because it makes you feel better, but does it help long-term? It feels good because we are stimulating the stretch receptors within the soft tissues of the back.
Let’s consider why the muscles are spasming in the first place. What if the body was naturally protecting itself against the expansion of a disc injury?
What if you had a fracture of the spine? Have you ever considered stretching is the wrong thing to do regardless of how it feels when you are done?
Everything that feels good is not good for you. Anyone reading this ever done heroin?
I haven’t, but word on the street is it feels incredible but really not good for you!
So, when is stretching okay?
It’s okay when we are dealing with an actual tight muscle, but when we are dealing with the “feels tight” type of tight, we need to consider neural tension. Neural tension is different than muscle tension and is treated slightly differently.
Do not stretch neural tension, as it will result in more pain. Some findings of tightness around the back are from neurogenic tightening. (Waterbury, T-Nation 2017).
Stretching will still feel good, don’t get me wrong, but this feeling of comfort comes from stimulating the muscle’s stretch receptors. The “feeling of tightness” is prevalent with many types of back pain, but can be secondary to the actual problem.
An example is a disc injury. Stretching of the muscles around the disc injury will make the area more susceptible to damage and bring more pain in the coming days. If you are unsure of what you have, you need to see a sports medicine specialist. Even though your first thought may be to start stretching your back out, you should think twice.

Even though your first thought may be to start stretching your back out, you should think twice.
More and more evidence has come to light showing that more flexibility in the lower back is not the answer, at least not in the short term. Sure, oftentimes, it can make you feel better, but does it address the issue?
We’ve already discussed that most people with a history of back pain are more than likely going to have more back pain in the future.
Perhaps that is because many people don’t address the underlying issues in the first place?
I was under the impression that maybe half of all people with back pain seek care, but was startled to read in one study that only 28% do! The exact number was 301 out of 1071 people experiencing back pain sought medical attention of any type (Mannion 2013).
Come on people! No wonder past injury results in future problems. Realistically, the underlying issue was probably never corrected. Your spine never learned to keep its composure during normal, everyday challenges.

Now, let’s get back to the flexibility topic again.
Is it OK to stretch your hips or hamstrings?
Most people default to their hamstrings and feel better after, but are there real reasons to do this?
I would vouch for hip stretching more than stretching the back, but mainly to improve functionality of the hips. Improving the function of the hips has been found to assist in saving the back from sustaining repeated microtrauma.
Back in 1996, we found back pain patients actually had the same amount of forward flexibility of the hips and back as people without back pain (Esola 1996).
Why is this significant?
Flexibility was not the reason for back pain. It was how people used their hips to save their back the work.
People with back pain bent their backs forward sooner than those who didn’t have back pain.
VIDEO COMING
Stretching the hips was suggested to assist mainly in getting people to move their hips sooner in motions, rather than their backs.
For this reason, I stand by stretching the hips as a way to improve hip usage in bending over, squatting and lifting objects. Using the hips well allows the back to be used as intended: as a rigid tube, resistant of bend.
Gaining motion in the hips can greatly assist in combating and preventing back pain.
Why?
Mobile hips allow the spine to remain in the correct position. Back injuries usually don’t occur from singe incidents. They occur over time or repeated deviations from midline.
The core/trunk functions as a spring. It wants to stand upright and will resist deviations from midline, but the issue is the eyes always win.
What do the eyes have to do with anything?
Just walk around and observe people. 99% of everyone you see (if they are not texting and walking) will look forward when walking. Both of their eyes are always even.
You will almost never see someone walking with their head tilted to one side.
You will almost never see anyone walking with his or her eyes/head looking up.
I say almost because I’m sure there will be one person who breaks the rule.
The eyes matter because no matter how the spine is tilted from the base, no matter how twisted and curved it is, somehow the eyes are always straight and even.
Proper hip mobility and pelvis function will allow the spring to have a proper base and then the eyes will do the rest.
I know there are so many ways to stretch the hips, so what kind of stretching do I recommend?
Dynamic or Active Stretching has been shown to have more beneficial effect allowing the nervous system to do its job.(Carvalho, 2012)
Passive stretching does deaden pain, but it also deadens the stretch receptor’s response leading to loss of functionality of that muscle, at least for a short period of time, such as using static stretching as a warm-up to sprinting.(Fletcher 2007)
Deadening the ability of the hips to do work leads to less strength, power and speed, which could lead to a back injury.
How does this matter if you don’t care about strength, power and speed from the hips?
You still need the hips to do work. You need them to stand from a chair, to pick up your son or daughter and to do cardio. Athletes just need their hips to work better…period.
Nobody should expect a healthy back without functional hips.
Still hanging onto the concept of static stretching?
When in life do we ever move by having someone else move our limbs under no strength of our own? I can’t think of one, unless you are training to be in a wheel chair, bed-ridden or a stand-up improv comedian. (Think Who’s Line is it, Anyway?)
Am I saying we don’t need hip flexibility?
No not at all. I’m just saying there is not a need to move any joint through range of motion if we don’t have the ability to control it through that range of motion. If you want to attain extreme range of motion (for some odd reason), I would suggest doing so with active or even assisted stretching, but not passive.
If you still insist on passive stretching, then at least spend some time actively going through that new range of motion immediately after.
If you don’t believe me about the importance of active hip range of motion in relationship to back pain just try this hip mobility exercise (ask your doctor first). Many of my patients feel over 50% better immediately after doing these with good form. Enjoy
Other Important section (click links to read immediately):
MYTH 3: CORE TRAINING IS JUST A FAD
MYTH 3: CORE TRAINING IS JUST A FAD
When I first began training my core, I thought how cool it was going to be to have a killer six-pack, but as I began to learn more, I found the core is actually on the inside. Unlike your thigh, the core is actually a hollow tube. The rippling muscles of the abdominal area are just the walls.
The core is what I like to call the body’s keg, like a beer keg. It has a top, bottom, sides, and internal pressure. Your belly region is the same. It has a lid, base, sides/ hoop system, and internal pressure that buts up against the spine from the front side, acting as a buttress system. It is EXTREMELY SUPPORTIVE, and when well-conditioned, lower back pain and sciatica improve very quickly.
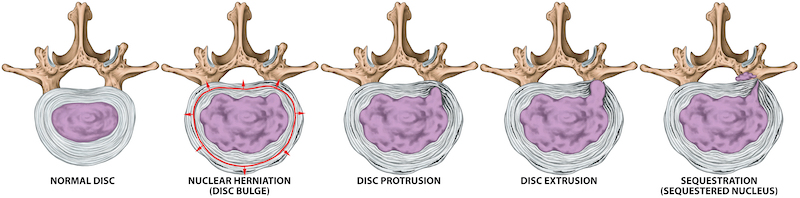
Most people get that the abs, back, and sides are included within the core, but I often lose people when we talk about the internal pressure. For this explanation, I tell them to consider a balloon, like the kind clowns, turn into balloon animals. The muscles would become the elastic of the balloon itself, yet we can’t ignore the importance of internal pressure.
The reason a balloon dog can even stand up at all is because there is pressure inside the balloon. Try to make a dog from a deflated balloon; it’s impossible. I’ve tried.
For a human, the internal pressure is produced by the diaphragm, pelvic floor, and abdominal wall, the sides of the beer keg. The whole loop is complete as the muscles of the spine contract to keep the spine in place. Yes, I meant to include the diaphragm/ breathing muscle.
You may be wondering how you could control your “breathing muscle?”
Just like your hamstrings, the diaphragm is a skeletal muscle, which means it can voluntarily contract (Kolar et al., 2009). All skeletal muscle is capable of being contracted when you want it to contract.
The diaphragm has two functions: getting air into your lungs and stabilizing your spine for support during all types of posture, good and bad. We’ve found that the diaphragm can multitask. It can allow breathing and stabilize the spine at the same time (Kolar et al., 2010).
You can learn to do this as well.
Learning to have the diaphragm in a “lower position” permits the muscle to allow breathing while simultaneously keeping pressure inside the abdominal cavity high. A muscle of the abdominal wall also assists the diaphragm in doing this, the transverse abdominis.
You need to learn to allow the diaphragm to do both of it’s jobs at the same time.

When your core is firing on all cylinders, you may even experience the side effect of “super stiffness.” This phenomenon where all of the muscles of the core contract together to create more stiffness than any single muscle could alone (McGill, 2017). Contraction of the muscles of the trunk in unison allows you to stay free of pain in various postures and position your body could be exposed to in daily life or sport.
Rolling out of bed, exiting cars, lifting your children, putting on your shoes, and sitting soon will be all pain-free by creating a fully functional beer keg.
How long will this take? It depends, but many people can experience a dramatic decrease in pain within a month’s time. I experienced a 75% improvement within a week, remember?! It can be that simple if you’re willing to put in the work. Using the right daily rituals, many people are surprised at the results and upset they didn’t find it sooner. I said it was simple, not easy. You would have to put in the work.
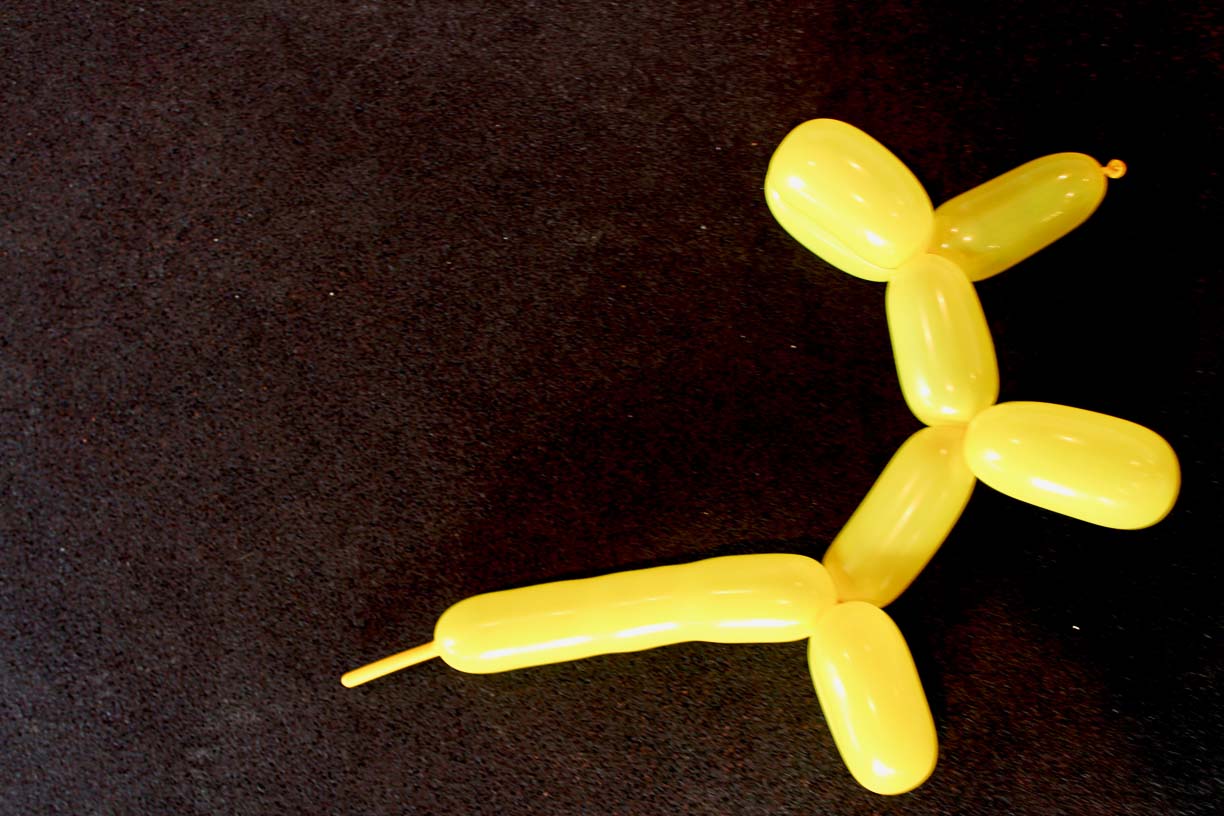
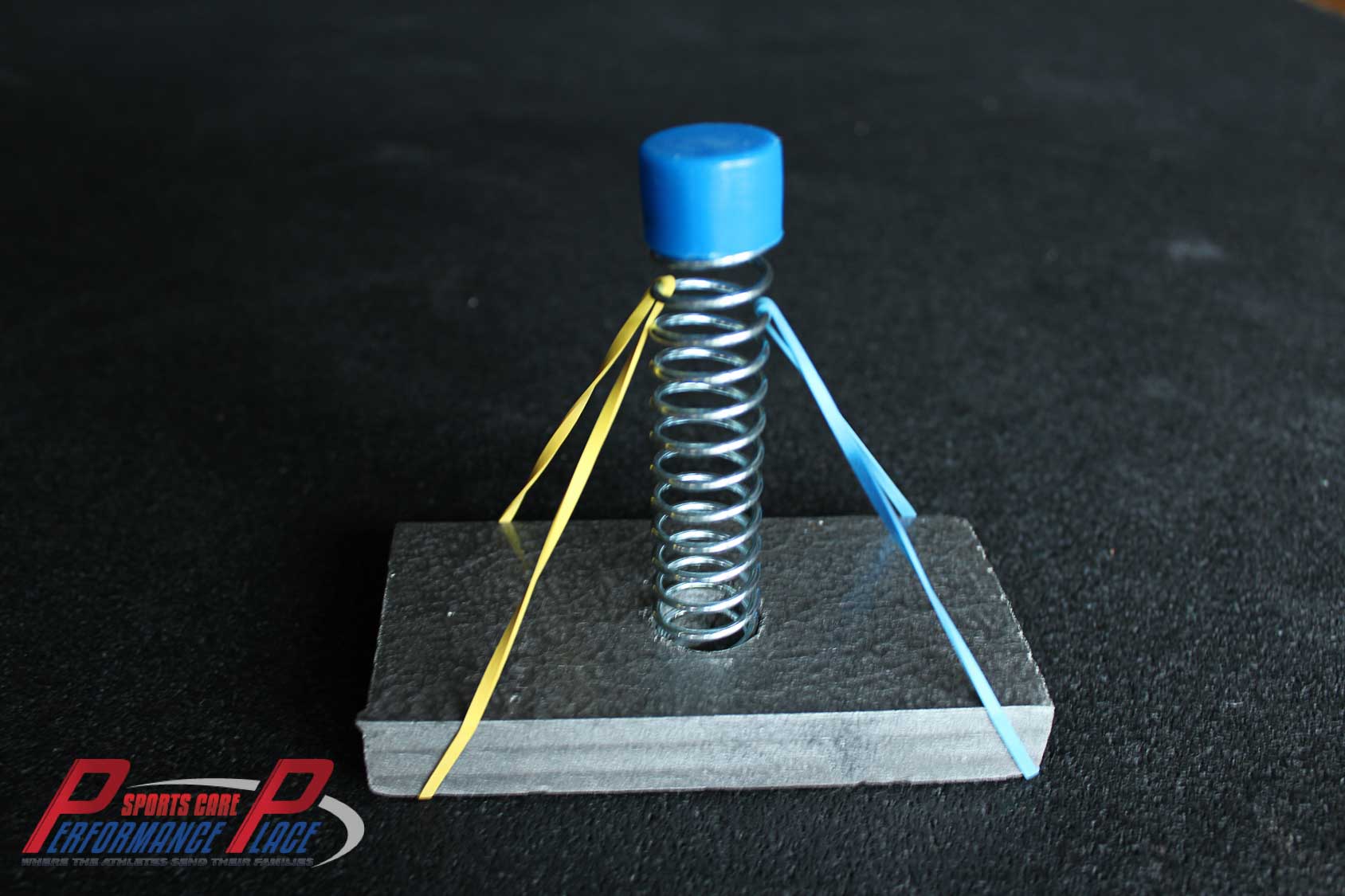
To demonstrate this beer keg co-contraction concept, I’ll like to draw your attention to the following images of the spring, the wood, and the rubber band system. Note: the only thing missing in this analogy to make it complete if we could put a balloon in the middle.
The more rubber bands we have on the “spring”, the better we will be able to withstand daily life. While this analogy paints a straightforward concept, in reality, it’s more complicated.
I have taken some pictures of a model I show my clients about the wireframe system. Note the image with a narrow contact point of the rubber band; the less leverage it has, the less support it gives the spring.
To recover from back and leg pain, development of high ENDURANCE of the human keg system is critical, and it may surprise you that when this system works together, it defies simple math.1+1 no longer equals 2. It’s more like 1+1=3.
Well, that math doesn’t make any sense! How does that work?
When working together, the trunk’s stiffness increases by leaps and bounds. And while each muscle individually may be capable of “X” amount of contraction, when working together, they are capable of more than “X.”
The internal pressure is the key. An excellent study in 2005 showed that there was an increase in low back stiffness (providing stability) as intra-abdominal pressure increased. Because this results in less aberrant motion of the spine, there are less lower back injuries and pain (Hodges et al., 2005).
Below, I placed some written instructions for the video exercise for you as well.
#1) Lay on your back, feet against the wall so your knees are pointed straight to the ceiling and your shinbones are parallel to the ground. Place your hands on your stomach and just feel your belly moving. If you don’t feel it, stay on the ground until you do. This is an important step.
#2) In the same position, depress your ribcage. If you don’t know how to do this, place your hand on the bottom of your ribcage, and practice making it disappear. Next, place your hands just under the ribcage and press in. Fight your hands with your trunk wall.
When breathing, you should feel the pressure INSIDE your core pressing back on your hands. The ribs will expand from all sides of your chest. You should not see your ribs flare, at least while practicing “filling the keg.” When practicing, it’s most beneficial to focus on expansion to the sides of your body. Attentiveness to the lateral expansion oftentimes results in better 360-degree motion, which is a sign of developing internal pressure.
If you have heard the instruction “bring your navel to your spine,” then you have heard of abdominal hollowing. The current thought is that hollowing is out, and bracing is in (Koh et al., 2014).
Why is hollowing out?
The current thought is that of a guy wire system holding the spine in place. Hollowing narrows the wire contact point creating less support than a full contact, which is, in essence, what happens when you brace. Hollowing narrows those supports, but the use of these cues for breathing certainly is helpful in specific circumstances.
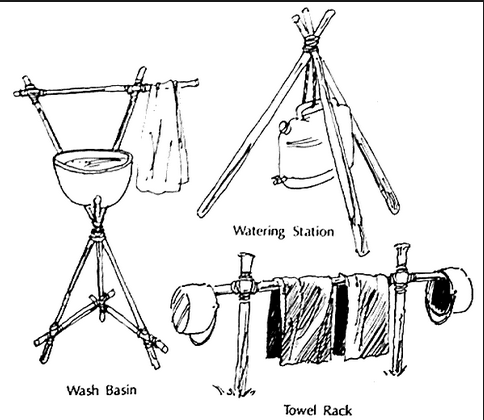
Growing up in Boy Scouts, we were required to make tripods for our water at camp, and we eventually found the broader the base of the tripod, the more stable it was. Healthy spines have a wider base. Don’t sabotage your spinal health by making the base narrow.

Dr. Stuwart McGill has suggested a baseline of these three exercises while using abdominal bracing and proper breathing to effectively stabilize the lumbar spine (Run Waterloo 2014).
The McGill “Big 3”
- Curl-up
- Side Bridge
- Birddog
We have full videos on them in our ONLINE COURSE HERE.
I would use these exercises to train the trunk to function better as it is intended. I don’t care about looking shredded or having a six-pack. As long as your trunk has the ability to retain an upright position through all of your activities, I would be happy.
The Curl-up
The curl-up is intended to train the front side of the trunk without having to go into flexion or extension the way you would with a sit up, a crunch, or even doing ab work on a ball.


If we take into account the true function of the trunk, this is a perfect exercise. The only downfall is some patients try to ditch it because of neck pain. Granted, there are corrections to make to diminish neck pain, so they just have to be utilized in order to keep this exercise in a program.
The McGill curl-up challenges the concept of “anti-extension”.
What does “anti-extension” mean?
Extension of the spine occurs when you are bending backwards like a “crab walk.” This exercise trains the trunk to resist extension.
Why do we want to resist extension?
In everyday motions, our spine likes to resist all extreme motions.
The goal with a curl up is NOT to flex at the spine.
During a proper curl up, we are attempting to keep the spine in a constant position during the entire exercise.
Here’s how we do it:
#1 Lay on your back with one knee bent and your foot flat on the ground
#2 Place your hands under the small of your back
#3 Subtly rise up off the ground, bringing your neck, head and shoulders off the ground (as if you are lightening a scale they are resting on)
#4 When raised, it is important to not lead with the chin or curl the neck (to combat this, form a double chin)
#5 Breathe through the belly
Hold for 10 seconds or until just before your form degrades and then lower
Alternate legs
Just like any other exercise used for the first time, the first time around can be used as a test to see if your injury will tolerate it. For this reason (at the very least), you need to see a healthcare professional to troubleshoot your condition.
Some corrections I often give are:
- Press through my finger (on sternum)
- Hover your elbows off the ground (stops cheating)
Progressions:
- Curl up with oblique pulling (fight my hand with your abdominal wall)
- Hold the top position for 10 seconds and breathe deeply
For correction of neck pain, McGill says:
Make the double chin and drive your tongue to the roof of your mouth HARD. The area under your jaw that was once soft will become hard.
The Side Bridge


The side bridge is not a side plank. Let’s get that part clear. It is more like a hip hinge with an anti-lateral flexion challenge.
With a side bridge, just as with the other “Big 3” from McGill, we are working on building the endurance of low-level trunk stabilization.
Here are the steps:
#1) Lay on your side on the ground
#2) Your foot position should be with the top foot in front. Your elbow, forearm and hand should be in contact with the ground. With your palm down, “press the ground away”.
#3) Your feet and your forearm should be inline. Your hips will be just behind them in the resting position. Think of this exercise as a forward-backward motion, like squatting, not bending.
#4) Top hand on your hip
#5) Drive the hips forward to “raise” the body up, just as in squatting.
#6) In full contraction, everything should be inline: head, neck, spine, shoulder, hip and foot.
#7) Hold for 10 seconds and slowly “sit back” into the starting position…everything should be under control as if you were deathly afraid of reinjury…in some cases this could be true.
Again, this is a test before it can be recommended, so be examined first.
These would be considered regressions from the one I showed:
Regression #1:
Depending on the person’s ability, we may not even start them on the floor. Standing and leaning against a wall in the plank position is a great starting point if that is all they can do.
Regression #2:
When first going onto the ground, we can start from the knees. Sitting the hips down into a squat position.
Shoulder pain?
Use the topside hand to press downward on top of the shoulder. Do not roll over to accomplish this.
Progressions:
#1) Wall lean
#2) Floor knees bent
#3) Floor knees straight
#4) Oblique Rocks (pelvis & ribcage stay connected…don’t lead with the butt)
#5) Rollovers to alternate sides
The Birddog:


The Birddog is a great exercise for multidirectional stabilization.
Here are the steps:
#1) Go on your hands and knees; shoulders and hips should be directly over your hands and knees.
#2) Find your low back neutral (go up, then down, then up to half way).
#3) Exhale and compact the trunk
#4) Pack the neck by making a double chin
#5) Pack the shoulder by pressing the ground away.
#6) Start with the arms: reach one arm out like you are superman. Make an angry hulk fist and contract the entire shoulder and upper back. Then do the other. All parts of the low back, mid back, and neck should remain still. Imagine you have a cup of hot coffee on your back…don’t spill it.
#7) Next, drive one of your heels straight back, making yourself long. Don’t raise it to the sky. Look for changes in the spine or rotation of the hips. Your pelvis should be facing flush to the ground at all times.
#8) 10 second hold at the top, come down and sweep the floor.
Progression #1:
Arm leg opposition at the same time.
Progression #2:
Make symmetrical squares at the same time with the heels and fist. Up, out, down, and up.
Progression #3:
Pop up using the hips and shoulder at the upward part of the square. Don’t use the back.
Regressions:
We can make this easier if there is pain or inability to perform it perfectly. Instead of raising the limbs all of the way up, we can just raise up part way or change the range of motion.
Other Important section (click links to read immediately):
MYTH 4: BACK PAIN ONLY HAPPENS ONCE
MYTH 4: ONCE BACK PAIN IS GONE, IT IS GONE FOREVER
Having pain in your past is a predictor of future hurt.
Does that mean if you have bad luck once with your spine, then you will have bad luck forever? Not at all, but you should be aware if you rehab it the correct way now, you will have fewer issues in the future, probably with less severity as well.
Are there factors that will increase the probability of your back pain in the future? Yep, there are. Psychological distresses in your younger years (early 20’s) and continued smoking have both been found to more than double your risk of having back pain.
Here’s a shortlist of psychological factors contributing to early back pain:
- Job dissatisfaction
- Lower education level
- Moderate to little life control
- High level of ergonomic stress, i.e., repeated “postural loads.”
- Single parenthood
Does this mean back pain is linked to your happiness? Maybe, but this does seem to indicate that people with a lowered quality of life report to the doctor with back pain in their early 30’s more often (Powers et al., 2001).
Does this mean back pain and sciatica are in your head?
No, but having a positive mindset, being happy about small successes, and having faith in your plan of attack is a great way to start.
Is there anything measurable to predict back pain?
We can use the flexibility of the back and endurance for something more objective. Increased back flexibility and low endurance of the spinal erector muscles have been shown to increase the possibility of first time back pain cases (Biering-Sorensen, 1984). Muscular endurance is a predictor of future low back pain as well (Alaranta et al., 1995).
Go back to these points and reread them, please. Note that the MORE spine flexibility you have with less endurance to control it, the higher your risk of having your first injury.
Interesting, huh?!
But, we can’t forget the quality of motion is also an essential factor. In my clinic, we spend a lot of time teaching high-quality motion to spare the spine and the nerves of the spine. Often complete concentration is needed in this reeducation of movement to correct these motor control errors. Research has found that even just being distracted can negatively affect the quality of motion (Brereton & McGill, 1999).

Other Important section (click links to read immediately):
MYTH 5: DEADLIFTING IS BAD
MYTH 5: DEADLIFTING IS BAD FOR YOUR BACK
Deadlifting is one of those exercises that scare people with “bad backs.” Rightly so, but if you have read to this point in the book, you should see by now that motion and how you use your lower back a critical factor in preventing a flare-up (Marras, 1995).
Think of deadlifting as training for real-life tasks. Deadlifting is the most efficient and safest way to pick up a child or other heavy object you encounter in your life, in many situations. Yet if you have been steering clear of deadlifting, this can leave your spine exposed to injury simply because it is currently unprepared. Note unprepared is different than being broken.


Even picking up light objects can hurt your lower back if you don’t know how to use your body. Education in maneuvering your body weight, as well as kettlebells, dumbbells, and barbells, are like re-reading your body’s owner’s manual.
In my clinic, we expose our patients suffering from lower back pain to some or all of these objects. Some of these people are afraid of “weight training” objects.
To address this, we’ve started to collect a library of more familiar objects they are not scared of, such as backpacks, purses, water bottles, and more. In some situations, the inert objects weight MORE than the dumbbell, funny what fear will do to a person. I get it, I’ve been there too!
Weights in our clinic are used to simulate objects you’ll encounter in everyday life. Heavy bags of groceries is 25 lbs. A Golden Retriever is pretty darn heavy too (75 lbs. or in my sister’s case 100 lbs.) Trips to Costco Wholesale result in boxes and boxes of bulk priced goodie!
I have a friend who just recently got into lifting weight. He has turned to an absolute maniac about it. One day he showed a video of his new personal record deadlifting to a co-worker.
This co-worker wasn’t into lifting and watched the video in horror. He asked my friend, “Why are you lifting so much? I feel like you’re going to hurt your back. My friend is a pretty logical guy, so he said, “I’ll never stop deadlifting. Deadlifting is life.”
What he meant was he would encounter a “deadlift” of varying loads every single day of his life. He wants to be able to do it safely every time.
Now, back to my commentary.
Is there a need to deadlift a ton of weight? I don’t think everyone needs to be able to pull double their body weight. Still, they should certainly be able to do above 75 pounds from an elevated platform (about 9 inches from the ground). Children weighing as much as 50 pounds can still want to be picked up.
My dog needed help in my car. She weighs 72 pounds. Personally, the most weight I’ve ever deadlifted was 300 pounds, but I lift more than half of that weekly. I want to be able to dominate any deadlifting challenge I encounter in everyday life.
Still scared of deadlifting? There is a way to mitigate your risk.
The Biering-Sørensen test is a great way to screen a possible injury from deadlifting rehab. If you can’t hold this test for 1 minutes then you need to start building your anti-flexion tolerance before you deadlift (Berglund 2015).
The second best way to predict an injury is simply pain intensity. If you hurt then you are going to get hurt. Duh.
I bet you’re wondering how to deadlift safely with back pain now?
It all comes down to proper cueing. Here’s a video on some of the cues I like to use. You should really just subscribe while you’re on Youtube.
Here’s some written deadlifting form tips:
The Deadlift Technique
The deadlift is an extremely important motion so even if you are hesitant to deadlift, I would really dig deep and understand the hip hinge so you can do it well. There are many reasons why people refrain from deadlifting (even light weights), but they are all bogus minus a few extreme conditions.
If you do have a condition, ache or other injury that you feel prohibits you from deadlifting, then you need to have it assessed by a qualified, medical professional to ensure that doing this exercise is safe for your condition. Run this by a few sports docs to get a good, honest answer.
Why do I teach deadlifting?
Here’s a short list:
- To rehab back, hip, knee and ankle injuries
- To improve sports performance
- To prevent sports injuries
- To build a strong core, strong hips and reinforce good, quality motion of the hips to save the spine from injury
This is going to be a very long section. I cut it up into sections of the lift, but you need to watch the entire video… probably multiple times to get all of the nuggets from it.
Deadlift responsibly.
Here are some verbal cues I often give people. I’ll go over them again so remember which ones your body responds best to.
Deadlift Cues
- Bar on the shins
- Pull yourself down to the bar
- Break the bar or show me the big logo on your shirt
- Drive the ground away
- Hips high
- Pull the bar into your hips; drive your hips into the bar
- Look 3 feet out in front of you
- Tension the bar, take the click out of the bar
Deadlifting: The Breathing and Bracing
I may be getting way ahead of myself, but core stabilization or what we call “rigidity” is one of the most important parts of proper/safe hip hinge motion.
I have all of the steps to this in the “Core” Section of our courses. The ones I would watch and master before you even attempt gripping the bar in a deadlift are:
- Breathing/Bracing
- Lewit
- Deadbug Progression
- Curl-up
- Side Bridge
- Birddog
- Pallof Press Anti-Rotational
To obtain proper breathing and bracing during a deadlift, we need to keep a rigid trunk by maintaining high intra-abdominal pressure throughout the entire lift; and that includes putting the bar back down.
Deadlifting: The Stance and Grip
Stance is typically the feet shoulder width apart with the knees stacked over the feet.
Hand position is best just outside of the shins.
For grip, I like to use a full palm contact when learning. Gripping with the fingers is a no-no.
The hook grip is the best option. People tend to use it when they are starting to lift heavier weight.
The hook grip is accomplished by wrapping the thumb around the bar and then wrap your fingers around your thumb.
Does it hurt? Yes, but you will get use to it just as the rest of your body does with training.
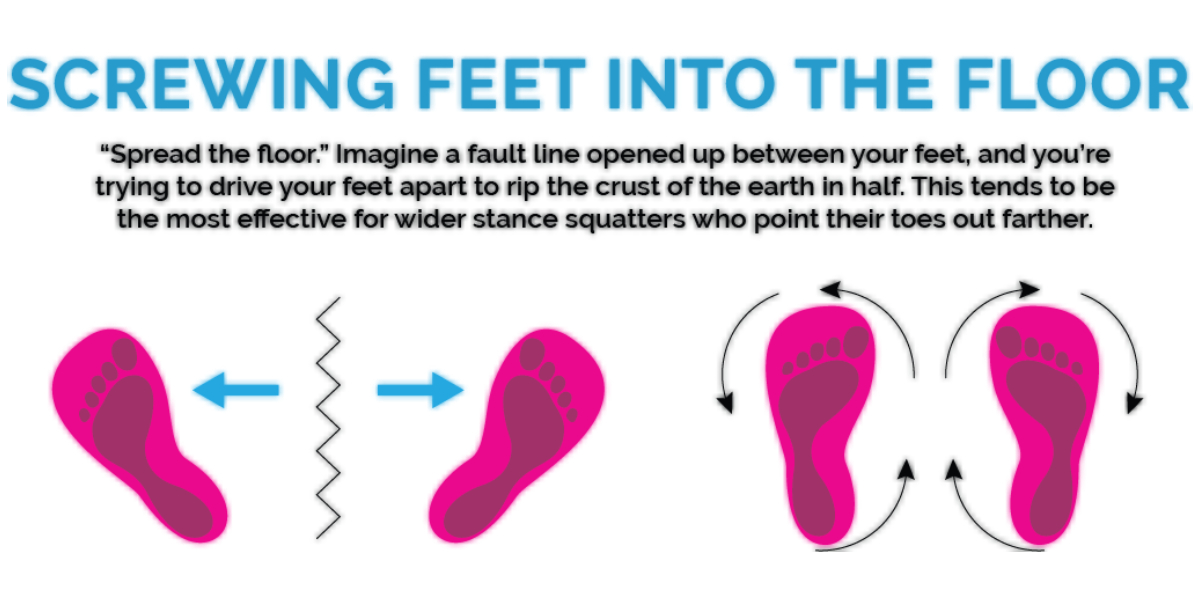
Also try this cue. Spread the floor. Using the stance and cue to tension the floor your glutes should “turn on” before you lift the weight.
Deadlifting: The Set-Up
Let’s go over some set-ups. The first two are ones I teach in person at our clinic, but there are many other ways. Different systems work for different people. It’s all about what your body responds to best.
Set-Up Option 1: Pulling your Chest to the Bar
I find this to be one of the best setups for beginners in the hinge pattern. I strongly encourage this one because we can use the bar’s weight as feedback to pull the back into a “flat” or “extended” position. I find if we focus too much attention on the hip height, then people tend to round their spine, which is the last thing we want.
- Bar on the shins
- Squat down to grab the bar
- Break the bar/Pull yourself down to the bar (to pull the chest through)
- Breathe and brace
- Raise the hips (tension in the hamstrings)
- Pull
Set-Up Option 2: Rock the Hips
I find beginners have trouble with getting off their toes. In lunges, squats and deadlifts, many will creep onto their toes like a “smooth criminal”.
To get them to feel the weight shift in this setup, we have them start more “over the bar”, which will put their weight onto their forefoot. With the “Rock,” we use the bar as a counterbalance. This builds trust that they can start bringing their weight back to the center of their foot.
- Bar on the shins
- Goodmorning to get to the bar and bend the knees (your weight will be on your forefoot and your shoulders will be in front of the bar)
- Breathe and brace
- Break the bar and rock into the hips (your weight will shift to the midfoot)
- Pull
Set-Up Option 3: Rolling the Bar
- Bar 3-4 inches in front of your shins
- Bend down to grab the bar
- Breathe and brace
- Roll the bar towards you, pull your chest through and drop the hips as the bar rolls
- Pull when the bar reaches the shins
Set-Up Option 4: Dip, Grip and Rip
Very simple and practical once you have extensive experience and have achieved proper technique. By extensive, I don’t mean being able to lift a lot of weight with poor form.
This is a popular technique, but it is used to get outside of your own head. There are no external cues which makes practice perfect. We are in the market to teach proper motion, not to crush weight with poor form.
Deadlifting: Before The Pull
I recommend “tensioning” the bar before we actually pull it off the ground. You will typically hear a “click” as there is a slight amount of room between the barbell and the weights attached to the end. It’s actually the extra room to get the weight on and off the bar that we are looking to eliminate with “tensioning”.
Tension the bar, hear the click and then bring the bar from the ground.
Why does this matter? Jerking the weight off the ground will create an “impulse” when the unweighted bar contacts the weights.
This sudden impulse can create injuries to the components of the spine… it’s like pushing someone when they aren’t ready for it versus telling them it’s coming.
Engage The Lats or “Break the Bar”
I touched on this earlier, but the reason to do this is to engage the lats. We want to break the bar by “driving your elbows back” towards the back of your body, but you need your elbows to be locked. That means no bending your arms.
Engaging the lats is important from a safety standpoint. The lats wrap around the low back and when engaged, they actually prevent it from rounding. This is what we call the “lat sling”.
We have some exercises we use in the preparation stages of the loaded deadlift to emphasize the use of the lats. Yes, it is actually that important.
Deadlifting: The Pull
Now that we have obtained pinpoint accuracy on the:
- Breathing/Bracing Component
- The Set-Up
- Tensioning the Bar
- Engaging the Lats
We can start to lift the bar from the ground. By the way, if you have not mastered all of those components, just go back and practice them for the next few weeks. Getting to the setup and tension can be tiring when done over and over again. Let’s get all of the necessary steps down pat before we attempt to pull the bar.
Don’t think “lift the bar.” In fact, ignore the bar and focus on these cues:
- Chest up
- Drive the floor away
- Drive the hips towards the bar
The Speed
If you’re wondering how fast you should be bringing the bar from the ground, it is different based upon your lifting goals.
For beginners, I suggest a lower speed when going from the ground to just above the knees.
When the bar is above the knees we drive the hips forward aggressively so it becomes a quicker motion.
Deadlifting: The Finish
Now that you are standing up tall, you need to be aware this is not a passive position by any means. I always tell people you should be ready for “photo day”. You should be as upright and tall as a statue.
- Crush the quarter between your cheeks
- Hold paper under your armpits
- Stand tall
Deadlifting: The Descent
Going back to the ground with the bar is exactly the same path as we came up.
Some common faults are:
- Squatting the bar down (This will look like you are forming a shelf for the bar at the knees).
- Reaching for the ground (This will look like you are rounding your back). I tell people to let the ground come to you.
As a side note, squatting is also very healthy on the lower back but form is an issue for many people. The slang “butt wink” at the deep portion of the squat is a sign of poor form under load.

Other Important section (click links to read immediately):
MYTH 6: POSTURE & USE HAVE NO CORRELATION
MYTH 6: HOW YOU USE YOUR BACK HAS NOTHING TO DO WITH AN INJURY
Quality of motion is more important than flexibility. I went over this in the above section on flexibility.
When lifting weights, your spine should be able to keep posture and remain as “stacked as possible.” Training the skill of rigidity and resistant of bending, assist in this scenario. Remember, this is a loaded/ weight training/ lifting boxes type of situation. Keeping a stiff, rigid spine is not needed throughout all aspects of life, and it is certainly not healthy.
Ballet dancers have developed the skill of moving the spine and locking it into place through a high tension isometric muscular contraction. When you see them spinning on stage, they are stiff, yet bent. Try spinning a cooked noodle, and you’ll know that stiffness is still an aspect of a graceful art like ballet. Flexibility without control is a receipt for disaster. The keg and dolly system teaches this.
Understanding that the spine should be able to become stiff in various positions, and hold that position against outside forces (barbells and other ballerinas) is critical. People tend to think they should not move their spine again after having a few bouts of back pain; this tends to create other problems.
Frequently, I’ve encountered people with lower back pain being afraid to move their spine in any direction. They tend to believe their spine is incapable of moving without being subjected to further damage. They believe their spine is damaged, weak, and prone to reinjury.
The remedy for these types of people range based upon their willingness to trust in the process and trust me as someone who can guide them out of their predicament.
When unloaded, your spine should be able to move freely. There should be no catches, stabs, and shooting: no tight muscles, nor tweaks. The spine is a beautiful thing. It is capable of tolerating heavy loads such as with weightlifting athletes, and it can be graceful as in ballet.
As you build your spine ability to be exceptional at one aspect (ballet), you also can’t expect it to be world-class at the other (lifting.) But there is nothing wrong with being a Jack of all trades. Only the top of each sport is the Master of One!
I want to be mediocre at both of these aspects and just play recreational baseball. I’m 38, I won’t make the majors, and I won’t get paid to play. I want a little of both skills and, most of all, to be pain-free. You’ll have to choose for yourself.
Throughout everyday life, we encounter events where we need to lift, bend, and twist our body, not our back. If you’re moving correctly (with your keg and dolly supports), your chance of having a back injury drops significantly (Escola, 1996).
Now that you understand that your beer keg system needs to be worked on, we have to move that keg into the pub. The logical way is to use a dolly with wheels on it. Nice, greased up wheels. The wheels of the dolly in this analogy are your hips.
The hips are what I call the “human engine.” The hips are the engines that move you from one place to the other. The engine that gets you up from the chair walks your spine out the door and allows you to lift your own body against the constant resistance of gravity.
The way we train the human engine is through hip hinging, squatting, and loaded carries. These exercises will prepare you for what life throws at you.
As a side note, the shoulders are your other dolly system. Being ball and socket joints, they allow for lots of motion. We won’t cover the “shoulder dolly” in this book, but you can see it in action when someone is doing pull-ups. A stiff/ semi-flexible keg is moving underneath a smooth ball and socket joint. The hips operate the same from below.
Research reveals that people with back pain use their back earlier in motion than those who don’t. They are lifting with their spine, not their hips. They aren’t using their engines; instead, they are using their keg.
This yields a bent up, dented keg that has low ability to dispense beer. Again let me return to the idea that we are talking about under load at the moment. This conversation changes as the load decreases.
It’s ok to have some lower back motion as the load decreases. The act of putting on your shoes can have lower back rounding IF it does not create pain. Identification of what movements and loads can have more spinal motion may require some guidance.
People with back pain and sciatica are making their backs do more than what’s typically required. People who don’t use their hips will use their lower backs more (Escola et al., 1996).
So, how do you improve how you learn to move well?
How would you improve how you dance?
How you hit a baseball?
How you play the piano?
Practice frequently. Repetition is not the only answer. A phrase I remember one of my coaches growing up saying was: “Perfect practice makes perfect.”
Meaning: you need to be doing it right to make your practice reap results. We teach “perfect practice” in my clinic and don’t just send you home with a sheet of exercises.

MYTH 7: “I HAVE A BAD BACK”
MYTH 7: “MY BACK IS WEAK” OR “I HAVE A BAD BACK”
This section includes tough love.
Stop treating your spine like it’s broken. The majority of back and sciatica cases are not surgical and can get better with some instruction and training.
Yes, I know…you have arthritis, but that usually has nothing to do with lower back pain. I know this concept is hard to swallow. Let me explain before we go on. There are many different types of arthritis. In the past, we used to believe osteoarthritis (“old age arthritis”) of the spine created back pain. Osteoarthritis can be in many places in the spine. One type you could have is facet arthrosis.
Okay, now to blow your mind.
There has been no association found between facet osteoarthritis and back pain (Kalihman et al., 2008). None. So, when your x-rays, CTs and MRIs come back with the findings of osteoarthritis, arthroses, or degeneration, don’t get distracted. There are bigger fish to fry. Besides, after age 60, there is a 100% probability of having arthritis, but I’m sure you know people over 60 without back pain, right (Kalihman et al., 2008)?

Arthritis is only an issue when it’s severe. If I had to estimate how many back pain cases that I’ve seen with severe enough arthritis to merit their back pain, I would say it’s less than 1%. Most people have movement issues.
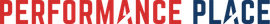
What about your disc herniation? It doesn’t matter. Disc extrusions and sequestrations are different conversations, but herniations tend to have a minimal relationship with lower back pain.
You heard me right. How did you get the disc injury in the first place?
Repeated poor motion creates more disc injuries than single incident trauma. Even small compressive loads (like sitting and poor lifting), when repeated, will damage discs, leading to herniation and prolapse (Callaghan and McGill, 2001).
Yet again, don’t get hung up on imaging findings. I have encountered far too many people afraid to try rehab because of imaging findings. A skilled spine practitioner doesn’t even need an image to start a trail of care. We start care with people all of the time without having X-rays or MRIs.
Many of these people are similar to me and feel better than they ever thought possible within just a few weeks. That is the power of DOING THE WORK and trusting your healthcare provider. Trialing care will not make your spine explode. It includes a small dose of movement medication that will reveal positive or negative information for us to move forward.
MYTH 8: GENETICS
MYTH 8: “MY MOM/DAD HAS A BAD BACK SO I WILL TOO”
This myth is one of the most common misconceptions I hear about back pain, and it is one of the most debilitating ways to think. Back pain has many different causes, and only a few of the major ones are hereditary.
There are situations where lower back pain has a hereditary connection; the individual creates much lower back pain we see in clinical practice. How you treat the spine your parent gave you dictates how you’ll feel. Mechanical low back pain is by far the most common type of low back pain. Since a significant aspect is mechanical, we all can improve how our back (and nerves of the spine) feel.


How your father destroyed his back in his younger years has nothing to do with how your back develops. Lung cancer runs in families, but the choice to smoke increases your risk substantially.
As far as the majority of lower back pain is concerned, do not blame it on your family. Your activities and how you’ve used your back throughout your life is the reason your back feels the way it does today.
MYTH 9: MRIS ARE NEEDED
MYTH 9: AN X-RAY & MRI ARE NEEDED FOR DIAGNOSING THE CAUSE OF BACK PAIN
Images of the spine are great to have if you do not lean on everything they say. X-rays and MRIs find normal, non-pain generating findings all the time.
A Meta-Analysis and Systematic Review in 2015, revealed a collection of data to suggest certain imaging findings were more significant than others when predicting low back pain. (Raastad et al, 2015)
Here’s a list of the ones that had a stronger affiliation:
- Disc space narrowing (working & community populations)
- Spondylosis (working & community populations)
- Spondylolisthesis (working population only)
Here’s some MRI findings that had weak correlation to low back pain:
- Osteophytes
- Endplate sclerosis
- Facet joint osteoarthritis
Why did these three imaging findings have less correlations than the prior three?
Researchers felt a possibility was that osteophytes, endplate sclerosis and facet joint osteoarthritis were “natural age-related” findings and basically happen to everybody at some point in their life.
My personal thoughts on this comes from clinical experiences. I remember a young Crossfit athlete who came into my office with severe lower back pain. He wasn’t able to tie his shoes, couldn’t sit for very long at work, or stand very long in one place without pain.
He presented me with an MRI that was 99% normal.
If I hadn’t been examining him personally, I would have thought he was faking. I can tell you this much…if he was faking, he was a REALLY great actor, and I’ll be booking him for my next blockbuster movie.
On a different note, I found it interesting that there was a weak correlation of back pain and facet joint osteoarthritis, which has been a long standing primary consideration as the reason for pressure on the nerve roots as they exit the spine through the intervertebral foramen. Apparently the nerve root could have a different irritating mechanism, structure or chemical process that is not seen on imaging.
Shacklock’s work, found in Clinical Neurodynamics, suggests that even light pressure on a nerve root can create neurogenic symptoms, via occluding venous return within the nerve itself. The arterial supply of the nerve has a greater pressure than the vein (as true with all other regions in the body) and will occlude with different pressures, essentially creating an increase in fluid within the nerve itself. (Shacklock 2016)
Now back to the imaging findings! Some examples of some findings you think are big deals, but may not be the trues causes of your pain:
- Osteoarthritis
- Degeneration
- Mild stenosis
- Small to medium disc herniation
- Scoliosis
- Spondylolisthesis (grade dependent)
There are many other big words that are used in imaging studies that don’t mean much when it comes to identifying the source of your pain. It’s like two mechanics talking about your car. Just because they used a word like “carburetor” doesn’t mean there is anything wrong with it.
The images also relay normal findings.
Oftentimes, the findings of x-rays and MRIs are not that big of a deal. They are not big enough to merit the type and severity of pain you are experiencing.
Does that mean you are making it up?
Not at all, but it should make you think about what the image doesn’t show.
If you can recall, in both of these images, you were asked to stay still.
These types of images do not show motion or how you move.
Here’s a list of things we look at as possible causes of pain NOT shown on imaging:
- Movement patterns
- Joint play or mobility
- Spinal muscle endurance
If you are anything like most patients, you want a definitive answer to what is causing your pain.
Rightly so, but be open to the possibility that your imaging is normal and your habits, the way you move, the way you sit, your lack of core stabilization, and/or hip mobility could be the reason. It’s not a diagnosis, but if you don’t believe it, go back to the smoking example.

Smoking constantly will yield a chronic cough…regardless of what a chest image shows you will decrease the chance of your cough if you stop smoking.
Constant poor motion and posture will yield back pain. The answer is to move better. This is why a majority of low back cases get better in therapy. Images are reserved for when you have a “red flag” in your case.
MYTH 10: IMAGES SHOW “X” AND THAT CAN’T BE FIXED
MYTH 10: “MY X-RAY, CT & MRI IMAGE FINDING CAN’T BE CURED SO THERE’S NO HOPE FOR ME”
As I noted in the section above, images do not hold the answer. Findings on images are often normal, non-painful, and can be left alone.
If we find a 2mm disc herniation, we do not need to have surgery right away. Since most back pain starts slowly and non-traumatically, chances are the herniation was there well before you felt the pain. If the herniation was there before pain, isn’t it rational to think you can be out of pain again regardless if it is still there or not?
Let’s correct the movement quality and increase endurance in addition to adjusting the possible activities that started the pain in the first place. If there is still no change after months of hard work on your part, then we can investigate the image findings some more.
Don’t be defined by the finding on your imaging test.
MYTH 11: POOR POSTURE HAS NO EFFECT
MYTH 11: POOR POSTURE WHILE SITTING HAS NO EFFECT ON BACK PAIN
Poor posture is one of the things I will agree with Grandma on, but her instructions on how to do it properly could’ve been better.
Sitting for prolonged periods and in poor posture will be the reason for many of your friends’ and family’s back pain.
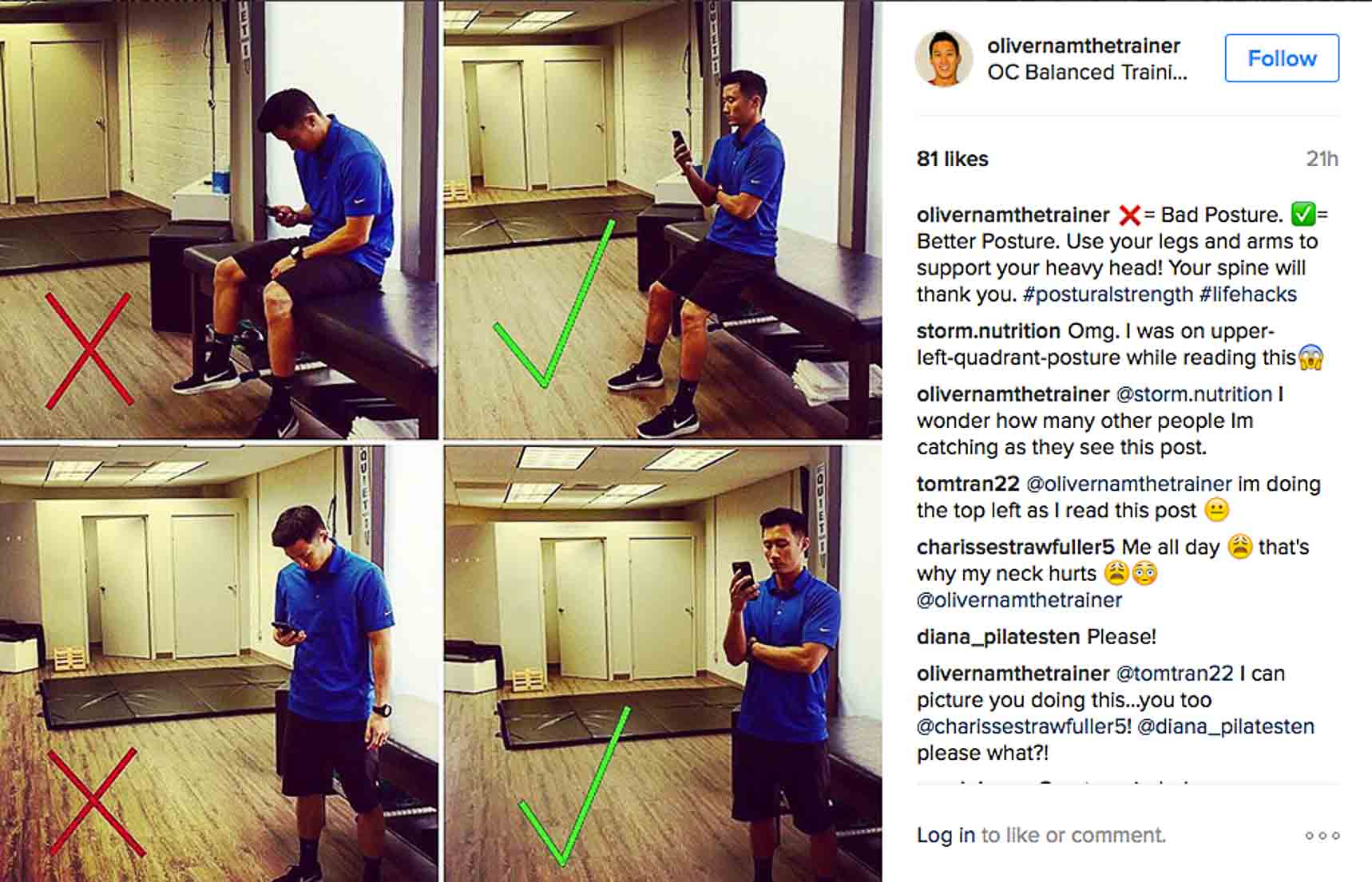
Poor posture leads to excessive compression on the discs of the spine and, eventually, the painful occurrences. Yet, this happens over years and years.
Everyone knows sitting can cause irritation on the lower back but did you know sitting with “proper posture” too much can create other types of pain?
You heard me right. Groin pain, outer hip pain, abdominal wall/ flank pain, and shoulder blade pain tend to occur when someone is “sitting properly” too much.
A simple suggestion is, move around. Too much of one position can create pain, even though it makes the lower back feel better. Move around. Go for a walk. Use a sitting desk for part of the day and standing for another. The reality is people with a standing desk end up having pain as well, from being stagnant too long. The short answer is to move!
Here’s the tough love again: I get it; many people feel chained to their desks. They feel like they are stuck with their back pain because of circumstances. Get creative and take your life into your own hands. Start to use your office space in a way where you can work in various positions and keep the high productivity your boss desires.
MYTH 12: BREATH IS BS
MYTH 12: THE WAY YOU BREATH HAS NO EFFECT ON BACK PAIN
That’s right, breathing the correct way does affect your back. Improper breathing patterns can increase the amount of pressure on different aspects of the spine, from the discs to the small joints.
You may be wondering what the correct way to breath is.
You have heard of chest and belly breathing before.
Chest breathing is when you see lots of ribcage and chest motion.
Belly breathing is when you see the belly move in and out, more so than the ribcage.
The current thought is we want to be belly breathing. We want the diaphragm to remain “low” in the abdominal cavity to keep pressure, and when contracting, we want it to move outward to the sides (Clare 2013).
Not up and down and not forward and backwards.
We can assess this by placing your hands on the bottom/sides of your ribcage. Close your eyes. You should feel the ribcage move towards your hands and you inhale deeply.
I would learn this lying down first, then seated and then standing.
Learning to breathe in this manner will allow your intra-abdominal pressure to shoot through the roof, protecting your back. DNS (Dynamic Neuromuscular Stabilization) practicing doctors suggest there is an easy, visual way to see if the core is engaged correctly. In someone thin or in-shape, if you see a dominant six-pack, then it is probably incorrect.
The abdominal area should be fairly convex, absent of the six-pack. If the six-pack appears contracted, then we have the possibility of an overactive rectus abdominis (Reinolds, 2012). In my clinic, we don’t always assess breathing in this fashion. Still, the utilization of breathing as a first-aid for lower back pain can start as soon as day one. Breathing homework is part of my lower back first-aid toolbox. It should be considered in your recovery.
I know that was a lot to think about since breathing should be an easy thing to do. Allow me to give you a few simple suggestions.
- Relax
- Give me a deep inhale and a slow exhale
- Breath deep into your belly
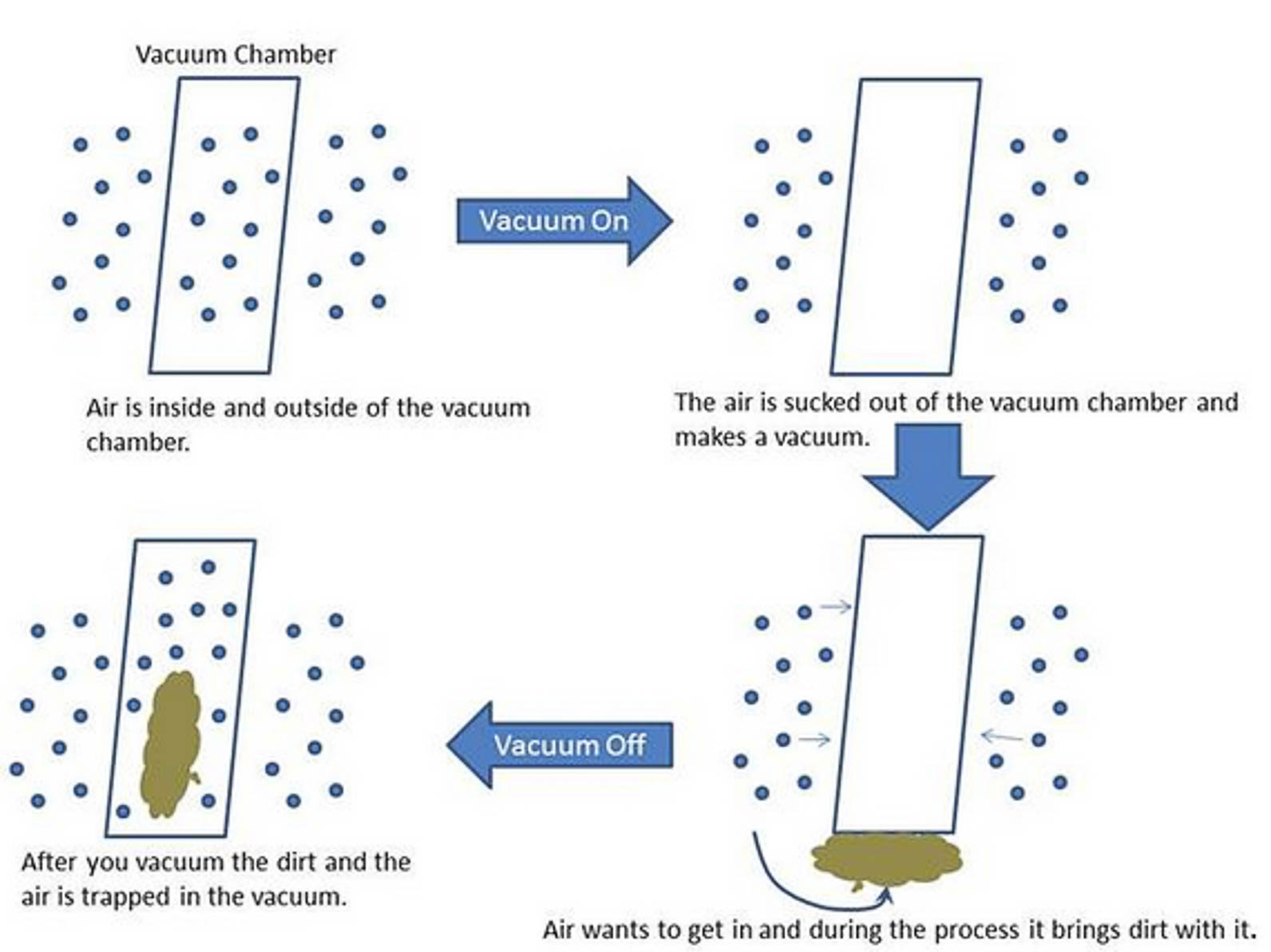
The diaphragm is the muscle used while breathing. Breathing occurs when the diaphragm contracts and depresses downward into the belly cavity. This downward motion creates negative pressure in the chest cavity, and the air gets “sucked in.” This is similar to how a vacuum works.
Vacuums create less pressure inside than at the outside, leading to “sucking.” If we reversed it and increased the pressure inside the vacuum, then it would turn into a leaf blower because the pressure on the outside is now less than inside.
MYTH RECAP & REFERENCES
I hope this was helpful to everyone. If you would like to hear more of me breaking down sports medicine lingo and thought processes, I have a podcast on iTunes. You can access it right here, and remember to share your favorite part about this article with a friend who has back pain and is sitting at home “Resting it off!”
Sebastian
Works Cited:
1. Hagen, KÃ¥re B., Gro Jamtvedt, Gunvor Hilde, and Michael F. Winnem. “The Updated Cochrane Review of Bed Rest for Low Back Pain and Sciatica.” Spine 30.5 (2005): 542-46. Web.
2. “Back to McGill.” T NATION. N.p., n.d. Web. 01 Jan. 2017.
3. Kolar P, Neuwirth J, Sanda J, Suchanek V, Svata Z, Pivec M. Analysis of diaphragm movement during tidal breathing and during its activation while breath holding using MRI synchronized with spirometry. Physiol Res 58:383-392, 2009
4. Kolar P, Sulc J, Kyncl M, Sanda J, Neuwirth J, Bokarius AV, Kriz J, Kobesova A. Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment. J Applied Physiol Aug 2010
5. Hodges, Paul W., A.e. Martin Eriksson, Debra Shirley, and Simon C. Gandevia. “Intra-abdominal Pressure Increases Stiffness of the Lumbar Spine.” Journal of Biomechanics 38.9 (2005): 1873-880. Web.
6. Koh, Hyung-Woo, Sung-Hyoun Cho, and Cheol-Yong Kim. “Comparison of the Effects of Hollowing and Bracing Exercises on Cross-sectional Areas of Abdominal Muscles in Middle-aged Women.” Journal of Physical Therapy Science 26.2 (2014): 295-99. Web.
7. Julia, Colin &. “‘THE BIG 3′ EXERCISES FOR YOUR CORE.” RunWaterloo. N.p., 18 Feb. 2014. Web. 02 Jan. 2017.
8. Power, Chris, John Frank, Clyde Hertzman, Gill Schierhout, and Leah Li. “Predictors of Low Back Pain Onset in a Prospective British Study.” American Journal of Public Health 91.10 (2001): 1671-678. Web.
9. Biering-Sørensen, Fin. “Physical Measurements as Risk Indicators for Low-Back Trouble Over a One-Year Period.” Spine 9.2 (1984): 106-19. Web.
10. Alaranta, H., S. Luoto, M. Heliövaara, and H. Hurri. “Static Back Endurance and the Risk of Low-back Pain.” Clin Biomech 10.6 (1995): 323-24. Web. 30 Dec. 2016.
11. Brereton, Lisa C., and Stuart M. McGill. “Effects of Physical Fatigue and Cognitive Challenges on the Potential for Low Back Injury.” Human Movement Science 18.6 (1999): 839-57. Web.
12. Mannion, Anne F., Simon Wieser, and Achim Elfering. “Association Between Beliefs and Care-Seeking Behavior for Low Back Pain.” Spine 38.12 (2013): 1016-025. Web.
13. Esola, Marcia A., Philip W. Mcclure, G. Kelley Fitzgerald, and Sorin Siegler. “Analysis of Lumbar Spine and Hip Motion During Forward Bending in Subjects With and Without a History of Low Back Pain.” Spine 21.1 (1996): 71-78. Web.
14. Marras, William S., Steven A. Lavender, Sue E. Leurgans, Fadi A. Fathallah, Sue A. Ferguson, W. Gary Allread, and Sudhakar L. Rajulu. “Biomechanical Risk Factors for Occupationally Related Low Back Disorders.” Ergonomics 38.2 (1995): 377-410. Web.
15. Berglund, Lars, Björn Aasa, Jonas Hellqvist, Peter Michaelson, and Ulrika Aasa. “Which Patients With Low Back Pain Benefit From Deadlift Training?” Journal of Strength and Conditioning Research 29.7 (2015): 1803-811. Web.
16. Kalichman, Leonid, Ling Li, David H. Kim, Ali Guermazi, Valery Berkin, Christopher J. Oʼdonnell, Udo Hoffmann, Rob Cole, and David J. Hunter. “Facet Joint Osteoarthritis and Low Back Pain in the Community-Based Population.” Spine 33.23 (2008): 2560-565. Web.
17. Callaghan, Jack P., and Stuart M. McGill. “Intervertebral Disc Herniation: Studies on a Porcine Model Exposed to Highly Repetitive Flexion/extension Motion with Compressive Force.” Clinical Biomechanics 16.1 (2001): 28-37. Web.
18. McGill, Stuart. “Core Stability: “Fascial Raking” to Stimulate Abdominal Wall Activation for Ultimate Performance.” Http://www.dragondoor.com/pdf/331.pdf. N.p., n.d. Web. 2 Jan. 2017.
19. Frank, Clare, Alena Kobesova, and Pavel Koh. “DYNAMIC NEUROMUSCULAR STABILIZATION & SPORTS REHABILITATION.” International Journal of Sports Physical Therapy 8.1 (2013): 62-73. Print.
20. Https://www.facebook.com/mikereinold.pt. “Core Stability From the Inside Out.” Mike Reinold. N.p., 06 Mar. 2012. Web. 30 Dec. 2016.
21. Fletcher, Iain M., and Ruth Anness. “The Acute Effects of Combined Static and Dynamic Stretch Protocols on Fifty-Meter Sprint Performance in Track-and-Field Athletes.” The Journal of Strength and Conditioning Research 21.3 (2007): 784. Web.
22. Carvalho, Felipe L.p., Mauro C.g.a. Carvalho, Roberto Simão, Thiago M. Gomes, Pablo B. Costa, Ludgero B. Neto, Rodrigo L.p. Carvalho, and Estélio H.m. Dantas. “Acute Effects of a Warm-Up Including Active, Passive, and Dynamic Stretching on Vertical Jump Performance.” Journal of Strength and Conditioning Research 26.9 (2012): 2447-452. Web.
23. Shacklock, Michael. Clinical Neurodynamics. Churchill Livingstone, 2016
24. Raastad, Joachim, et al. “The Association between Lumbar Spine Radiographic Features and Low Back Pain: A Systematic Review and Meta-Analysis.” Seminars in Arthritis and Rheumatism, vol. 44, no. 5, 2015, pp. 571–585., doi:10.1016/j.semarthrit.2014.10.006.
TRUTH 1: YOU WON’T BE ABLE TO HAVE SEX
What happens if back pain goes without rehab and treatment?
A few readers have mentioned that they wished they’d have known about the long-term effects of back health earlier in life. They said that if they’d have known what would happen, they would have taken better care of their backs.
In this section, I’ve decided to go down the “scare tactic” route. I’m going to tell you the top seven things that could happen if you never address back pain that occurs on and off over 20 or 30 years.
I’m usually not a “Debbie Downer,” but for the sake of motivating people, I’ll gladly play the part.
If you’ve had a bout of lower back pain, you know having sex is tough. Most people don’t like to talk about it, but will openly admit their difficulty when asked directly. When you have back pain, even small, unexpected motions can create sharp, shooting pain that can take you to the ground.
Intercourse is full of unexpected motions.
Patients surprise me weekly. If I had to estimate, one out of every 50 people with hip, back, and shoulder conditions openly tell me that intercourse with their spouse in the main reason for their treatment. The couple is frustrated, to say the least!
The way we address the back, in this case, is to start with teaching proper breathing. Proper breathing allows for an increased intra-abdominal pressure, which yields a torso that’s more resistant to bending. If you’re confused by this, we have a whole section in this article on the concept.
Most people think that as long as their back pain goes away, they have finished dealing with it. Wrong.
Past back pain starts a process of degeneration. Degeneration of the spine isn’t a huge issue; in the beginning stages, it’s often not even painful. Still, when it becomes severe, it often leads to chronic pain, injections, surgery, and disability.
Even that one week of back pain ten years ago can trigger the process!
How can we stop it?
By eating well, moving well, breathing well, and knowing how your body functions! If you can’t do all of those things, then there’s a strong possibility you won’t be having pain-free sex after the age of 50.
Here’s a video that can help- “Sex Positions that don’t hurt your back.”
TRUTH 2: YOU WON’T BE ABLE TO EXERCISE
Exercise regimes aren’t important to everyone, but when the structure of your back begins to degrade, you can kiss that morning run, lifting, or boot camp session goodbye.
Even without pain, the back degrades unless we choose to take the necessary steps to stop the process.
One of the simplest ways is to eat well. I interviewed Dr. Robert Silverman about this just recently. Here’s the podcast session:

A healthy back doesn’t happen on accident, and it isn’t genetic.
Do you love to Crossfit?
I’ve worked with many Crossfitters who are no longer able to run, deadlift, burpee, or kip because of the slow degradation of their backs. Most of them told me stories of how their back started hurting over 20 years ago, and it’s been on and off since.
Do you love to run?
The back is subjected to a rotational force when running that can increase chronic back pain. This rotational force increases as your pace increases. I have had many runners who had to change running partners, so they don’t feel like they are holding back their faster friends.
Could you imagine changing running partners?!

In the early stages of back pain, we can work on your ability to tolerate the rotational forces of running. Twenty years of spinal damage doesn’t make this process easier. Just like a house with termites, we could have stopped the decline with early treatment of the problem.
Do you love to do yoga?
Yoga requires the body to go through ranges of motion without pain. With chronic degeneration of the spine or spinal stenosis, some positions in yoga may not be attainable. Holding them will be impossible.
TRUTH 3: YOU WON’T BE ABLE TO LIFT THINGS
TRUTH 3: YOU WON’T BE ABLE TO CARRY SMALL OBJECTS WITHOUT PAIN (CHILDREN, GROCERIES, OR PURSES)
When the lower spine is healthy, it can tolerate side bend like a young sapling tree. But when the spine takes years of inflammation and degradation, it will flare-up with activities like this.
When rehabbing the spine, we teach each person to make their spine sapling-like again via specific, corrective exercise and therapy. Chronic pain responds much slower and often flares-up, leading to avoidance of the activities above.
Disability is “a physical or mental condition that limits a person’s movements, senses, or activities.” Avoidance of holding children or carrying groceries or bags is, by definition, disabled. Don’t be disabled. Develop healthy back habits before it’s too late.
Here’s a video on how caregivers protect their backs. Get some tips from those who lift kids all day for a living.
TRUTH 4: YOU WON’T BE ABLE TO TRAVEL
DRIVING, FLYING OR CRUISING
Sleeping in hotel beds will become intolerable.
Flying for even two hours can be unbearable.
Cruise ships may seem like a great option, but the motion of the boat can be excruciating for people with chronic back pain.
I’ve had a few people come back from cruises saying that their back, hip, or knee began to hurt after a few days.
If you plan to travel in retirement, you’d better start developing healthy back habits today. Even five minutes daily can be enough to slow the process of spinal degeneration. There is no reversing disc degeneration, so you need to have a prevention mindset. It starts with developing the right daily habits.
Here’s a great video on why your back hurts while on a plane.
TRUTH 5: YOU WON’T BE ABLE TO SLEEP
THROUGH THE NIGHT
Waking up every two hours because you’ve rolled into an uncomfortable position gets old fast. Restlessness in bed also creates tension between spouses.
Lack of sleep from back pain can also lead to dependence on pain medication.
Recently, a patient with lower left back pain told me he couldn’t sleep through the night, so he took one of his wife’s Vicodin. I was shocked! This guy lives a clean life — no drugs, clean eating, and infrequent alcohol consumption- yet he was willing to take an opiate-based prescription medication! Funny how the lack of sleep will change your habits so quickly. The statistics on this subject don’t lie:
– 37% of people with back pain say it affects their sleep
– 58% say they take prescription medication to deal with their pain
Dependency is real!
Just five minutes a day (the time it takes to get dressed) could prevent loss of sleep and a life of drug dependency.
This video has some great tips for Dos and Don’ts of sleeping.
TRUTH 6: YOU WON’T BE ABLE TO GOLF
TPI collected data indicating that 28.1% of all golfers experience back pain after every round. As we age, this percentage only increases.
Funny how that works, huh?
When we’re young, we don’t have the time or money to play golf, but we’ve got the body for it. In retirement, we have the time and money, but the body is no longer there.
Start developing healthy back and body habits when you’re younger.
Here’s a great video on back pain while golfing.
TRUTH 7: YOU WON’T BE ABLE GET OFF GROUND
OR PLAY ON THE GROUND WITH YOUR KIDS/GRANDKIDS OR DOG
Guess where children and dogs like to hang out…on the ground. They aren’t coming to you, so you have to go to them.
In chronic back pain cases, the natural motion of getting up and down from the ground can create muscle spasms and stabbing pain, leaving you lying in bed for a few days.
Training the body to control these motions will help a ton. Still, it took your spine years to degenerate so that it won’t return to perfect again overnight. Building a stable and healthy back is a process, not a quick-fix.
LOW BACK PAIN TRUTHS RECAP
It’s never too late to improve how your lower back feels. I’ve seen thousands of patients with back pain, and most of the people who don’t get better also are not willing to put in the necessary time and effort to feel better.
All lower back pain cases are unique in their own way, but a majority have similarities. When they follow The 5 Step Process of how to decrease pain and then build up a buffer, most people can live without excruciating lower back pain. The 5 Step Process can have slightly different exercises and homework, but the goals are generally the same.
The 5 Step Recovery System
Step 1: Proper Diagnosis
Step 2: Reduction of Daily Pain
Step 3: Building Endurance
Step 4: Building Strength
Step 3: Movement Variability
Steps 1-2 should happen very quickly, and pain should be able to be reduced within ten days from onset (if the treatment is correct). With inadequate treatment, this can take years. Many of you know friends who have been through this kind of failed care. Steps 1 and 2 are challenging to some people. Think of this as the effort to get an airplane off the ground in takeoff.
During Steps 3-5, you could be running and lifting weights. You should feel no pain, or very minimal pain, during daily activities. In Steps 3-5, the goal is to create a buffer to prevent re-injury so you can run as much as you want. Think of it like keep your airplane off the ground AFTER takeoff.
Step 3 takes the form of POSTURAL endurance. Building the entire body’s ability to keep posture while running, starts by using simple floor based rehab. These are useful for about four weeks before they need to be progressed into something more long-term.
Step 4 is “REAL REHAB.” Rehab is training while injured. This step takes the form of specific prescribed exercises that look like weight training. Body adaptations that occur in this step take a minimum of 3-6 months.
Step 5 is a playful, non-loaded movement. Generally, movement can be used as medicine, but we need more than just running as medicine.
This methodology can be applied to lower back pain, as well hip pain and leg pain. We have a video recovery guide available if you want to get started today.
Healthy backs, on the other hand, can be thrown into a more generalized category. The building blocks of back wellness can be attained in under five minutes a day. The next level requires us to allow time for exercise and weight training.
Thank you for taking the time to read this article. I put so much time and effort into writing. Allow me to help you recover from lower back pain. It will be faster than you ever thought possible and cheaper than surgery.

STUART MCGILL PODCAST INTERVIEW
Have you been dealing with back pain, stenosis, disc herniations, pinched nerve sciatica, or Fasset syndrome, there’s lots of different reasons for back pain, but what we often times don’t know is that they can often get a lot better, if we identify pain triggers in rehab, the torso properly, I’m having an interview today with Doctor Stuart McGill, who is one of the world’s leading experts on back conditions and how to rehab them, this is a video version of the podcast, don’t forget to subscribe, share with friends, and like this video, here we go. This is session number 67 of the Performance Place Sports Care podcast.

– [Narrator] Welcome to the Performance Place Sports Care podcast, where you can learn about sports injuries theory, rehab, diagnosis, and how to understand the Doctor lingo you didn’t understand at your appointment, and now your host Doctor Sebastian Gonzales.
– [Dr Sebastian Gonzales] Hi everyone, thanks for joining me again, I’m Doctor Sebastian Gonzales with the Performance Place Sports Care podcast, Barrel House is one of my favorite places, and if you know me pretty well, you know that Barrel House I get excited about it, Barrel House is a brewery, it’s in Paso Robles, California, which is a place where we spent a lot of time growing up, at least over on the coast side which is Cambria, so we went to Paso Robles again this is a brewery, we went there for the first time a couple of years ago, so I guess it was 2016, but we showed up and there’s the nicest people there, they tell you all about the community of Paso Robles, as well about the brewery and the whole region, and how it kind of got developed, and it was just nice every time we went back there there was just so many nice people to talk to, the beer is great, the ambiance is awesome, and it’s one of my favorite places, so if you ever get a chance to go there, just give a big Barrel House yell, and it’s a good time, so I don’t think you will be disappointed.
So in this podcast today I’m actually having a great expert on back pain or back biomechanics, his name is Doctor Stuart McGill, he is a professor of spine biomechanics at the University of Waterloo, he’s been on a fair amount of podcasts which I have shared with some of my patients, and I actually started to share the podcast that he was on with my patients with back pain, and the reason why I did this is because a lot of times if you work in this type of realm, if you’re a PT or Chiro, or you’re an MD, you try to explain back pain to people, or explain their injury, and sometimes it takes, actually a lot of time it takes sometimes to sink in, to really understand, and what I suggested to at least the first patient, I had listened to a podcast right there in the office, and I came back about 10 minutes later, and she basically said after about two minutes she tuned out, she just couldn’t pay attention, and it wasn’t that the topics were extremely complex with back pain, but it was just a little bit more than she could tolerate, and I thought I would ask Doctor McGill to come on, and we’ll answer all the basic fundamental questions that new patients ask about back pain, so part of the reason for this podcast here, this session, it’s kind of a selfish reason, because I really want people in my clinic to understand back pain, and I thought if I could have Doctor McGill come on and explain it, he explains it so well, he’s had so much experience in his labs and writing books, and he explains back pain in a very mechanical way, I think they would get it, I think they would have success in life, so that was the goal today, and I would strongly encourage the other doctors and these chiropractors, or people who don’t understand back pain, share this podcast with your friends or your patients who have it, because I can tell you how many times I’ve seen people, come in with back pain, and they’re extremely emotional about it, if we break this thing down, and when you hear Doctor McGill speak about it, we can mechanically break this whole thing down, it’s not an unknown type of condition to work with, we can figure this thing out, but a lot of people end up having lifetime medication, they have surgery, they have lifetime disability from it, it’s very frustrating for them, but we can figure this out, in the rare cases where we can figure it out, I think we need to explore malignancy, tumor, infection, or the large types of things, so if you’re experiencing back pain, are you have friends or patients experience back pain, I strongly suggest you have a listen to this podcast, we’re going into the most commonly asked questions, I might go a little bit deeper into some secondary level questioning, but all the stuff that has to do with the mechanics of the spine and the technical terminology, we’re going to try and leave that out, and it’s not to dumb the idea down or dumb the concepts down, but it’s to make it understandable to people, so they have an actionable process after, so we are trying to combat patient misunderstanding, and only have them do medications, pain killers, and injections when it’s actually needed, because a lot of times that is a really quick fix for people.
And before we go onto the interview, I want to remind people to go into iTunes and review, it helps a lot, I get a lot of feedback from that, but also to I want you guys to check out the other podcast, we have other experts on for other types of conditions, shoulders, knees, hips, ankles, even weight loss, and a lot of things sports injury-related, so my goal is to further educate patient populations, and if you are a healthcare provider, please share these with your patients, it will save you a lot of breath, and it will help them comply with their care much much better and get better faster, so here we go with the interview. Okay everybody here is our interview with Doctor Stuart McGill, Doctor McGill say hi.
– [Dr Stuart McGill] Well hello to all your listenership, and to you Doctor Gonzales.
– [Dr Sebastian Gonzales] Well thanks for coming on, I’ve really, really wanted to have you on for a long time, and not until, do you know Doctor Seth Meyers, he’s in Idaho, or Kansas?
– [Dr Stuart McGill] I know of him, absolutely.
– [Dr Sebastian Gonzales] He is actually on right before you on the podcast, so he spoke about a lot of your stuff, and I thought we should just have the master on right here. So I thought we would go over today some of the questions that first-time patients have on back pain, because from a healthcare site, or a clinical side, we see a lot of patients who don’t really understand back pain, and they are very emotional at the time, and I think sometimes explaining something logically and mechanically to someone who is a little bit emotional, sometimes we have to get really in-depth into education, I thought we go through these questions which we as healthcare providers get all the time, sound good?
– [Dr Sebastian Gonzales] Yes. So, first off is all low back pain created equal?
– [Dr Stuart McGill]You’re starting with the big philosophical questions first, well I’m going to give you probably a big answer on this, with maybe three levels, some logic, some examples. Let me reverse that a tiny bit and say well have you ever heard of non-specific head pain or leg pain, is leg pain created equal, I mean we don’t even put up with such a notion, it could be torn knee ligaments, vascular complaint, a cut or whatever, so this notion of back pain, it is so non-homogeneous, and what I mean by that is one person might have back pain because they’ve got a disc bulge, the next person might have it for an entirely different reason, so starting out with that logic and setpoint, all back pain has a cause, and if we can obtain a specific and precise diagnosis of the pain mechanism, then we can address it appropriately, so is it created equal, right off the top three contrasting examples of back pain come to mind, think of a person who is in their mid-20s, 30s, 40s, say they work sitting at a computer eight hours a day, sitting at the computer for 20 minutes gives them back pain, and yet they can stand up and go for a three or four mile walk and that would be therapeutic, now let’s take the next person who is newly retired, and they have more of a stenosis or arthritic mechanism to their back pain, and interestingly enough the precise opposite occurs, walking starts to cause back pain, and sitting down is relieving, and then I can give a third example, let’s take a young athletic team, you can take a football team or a baseball team, and when you study the back pain patterns you will see that they form cluster groups, for example one team might have four stress fractures on their roster, in their back, and those stressed fractures were not caused by baseball, it was caused by the strength and conditioning coach, who was getting them to do full range of motion loaded rotations, and eventually caused a spondylitic fracture, and maybe full-blown spondylolisthesis, so each one of those would have a different time course, a different symptom pattern, and really a very different strategy to address them, and as you know in my books, I give many more examples, but there is an example, one is a programming flaw, one is the person who sits and works at a computer for eight hours, and then goes to gym for one hour at night, and basically does a bodybuilding program, and wonder why they still have pain, had they reassessed the programming to really try and create an antidote for the common stresses of sitting all day, that would be a very different approach than the older adult. So if I could just leave that notion and finish of the answer on a more philosophical level, because I’ve already talked about the importance of obtaining a precise, diagnosis of the pain mechanism, you know that there is no provision in the current medical system to get a thorough assessment of your back, if the patient is lucky they wait for a while and get a 15 or 20 minute assessment of their back pain, now your practice is probably different than that, I set aside three hours when I see a patient, and we do provocative testing, to really isolate precisely the specific motions postures and loads that trigger their pain, all the time I’m assessing their learning style, so I know how to coach and get what I need from the patient, I let them talk freely and they tell me about the various impediments in their life that have prevented previous attempts to reduce their back pain sensitivity, from working. Et cetera, et cetera. So that is certainly, a huge impediment in the medical system, but what that produces is many clinicians who really haven’t been trained in the nuances and mechanisms of this broad spectrum of back pain, they will do some sort of non-specific treatment, to non-specific back pain, and they tell the patient there can’t be anything wrong with my therapy, therefore the pain must be in your head. And the patients I get, who failed different approaches, many have been told that the pain is in their head, and this is just a pure default of incompetent clinicians, I’ve had people, who were on the brink of suicide, they are very solid citizens, some doctor has told them that pain is in their head, when they know it’s in their back, and they can change the pain by doing different activities, or avoiding some activities, and it drives them to the brink of some of them considering suicide, so there would be a very iatragenic cause to pain with secondary issues as well, so there is a huge answer to a very huge question, I hope I didn’t get too far off topic, but I really wanted to begin with addressing this idea of just generic back pain, there is no such thing, it’s all specific and it needs to be sub classified and treated with precision and specificity.
– [Dr Sebastian Gonzales] Okay, you definitely didn’t throw me off topic there, there are a couple of things we’ll revisit a little bit there, so what I’m hearing is that first off, the majority of back pain has a logical reason, it’s mechanical, and it’s not in their head, is that what I’m hearing first?
– [Dr Stuart McGill]Well it does go into their head, when they have been told it’s in their head, and it drives them crazy, so that’s a little bit off at it depends answer, but generally speaking when their pain mechanisms are recognized, and they address them mechanically, the psychological sub issues can be resolved, but if all you do is treat the psychological through cognitive behavioral approaches et cetera, chances are that pain is going to come back to revisit them.
– [Dr Sebastian Gonzales] Okay, you said there is three kind of major categories, I guess we can differentiate back pain into, there was the young disc-based person, there was the older arthritic or stenosis, and then there was the special population athletic there in the middle, so each of them I’m guessing, they have different symptom patterns, within each collective group, let’s just start with A disk young kid, are all these people going to be the same, or order different subsets in their how they feel and how they respond and so on?
– [Dr Stuart McGill]Well I teach a master level course in assessment, and the theme is we get right down to a subject category N equals one, and what that means is there are no two back pain mechanisms that are exactly the same, so if we keep slicing it down, what is the magic dose to wind down the pain sensitivity, what is the precise exercise, the order, the dose et cetera, to build that foundation for a pain-free movement, it’s going to be slightly different, so you could have two people with exactly the same category, but they are in different positions in the program progression, one might be more advanced, so their program, you don’t just give a person a set of exercises and say go away, there you are, you will start by establishing movement patterns, that avoid their pain mechanism and wind it down, and then you might add some hip mobilizing patterns, and then you might add some spine stabilizing patterns, and then if they eventually want to play tennis, you’re going to have to add some footwork, but anyway you get the idea, when we’re dealing with the person in the thorough assessment, will slice it right down, so they are a category of back pain of one, themselves.
– [Dr Sebastian Gonzales] So as you know I wrote down a list of things to go through today, I’m going to jump around slightly, because I’m gonna go right down this path, with people since they have a very unique mechanism of injury, in a unique injury, how active or how much are they participating in their own resolution of their back pain, I know a lot of people go and they say I want this treatment, I want that one, can you stretch me out, how much do they have to understand about their back pain to make it resolve and not come back?
– [Dr Stuart McGill]Well I’ve already mentioned that most family doctors, if we were to take them as a clinical category, they could virtually nil training on what to do with patients who come in with so-called back pain, and when you speak with them, they will freely admit that they don’t know what to do with patients, so they end up giving what they know which is an analgesic pill, a pain pill, so because of that, I would suggest that the people become savvy, and advocates for themselves, now again I’m not trying to plug my stuff here, but that was why I wrote the book back in Canada, I had written textbooks for clinicians, so they were very heavy textbooks, I never envisioned 15 or 20 years ago writing a book for the lay public, but the lay public would read my heavy clinical textbooks, and say this is insightful for the first time we are learning about the real mechanisms of pain, would you write one for the lay public? So that is why I wrote Back Mechanic, to guide the reader through a self-assessment, obviously a simplified self-assessment, and then to discuss some of the controversies with them, And then it became empowering, they realized that they were accountable and in control for winding down their pain sensitivity, and building this foundation. So the answer to the question in a long about way is yes they must become participants and advocate for themselves, because no one knows their pain better than themselves, they just need a little bit of guidance and interpreting.
– [Dr Sebastian Gonzales] Actually I did mention to you I read a strong majority of the book, and actually the first page, I’m going to flip through real quick, it was a myth busting session, I thought it was amazing, and even the first part, I got a highlighter out and I started doing some highlighting on it, I think it was very, it was very empowering I think to hear that we are debunking these myths surrounding back pain, and I totally agree with you when you’re saying that you made the book for clinicians, but the general public they have a whole different leading level, and that’s not to sound insulting, it’s just they didn’t have the education in this stuff, so how are they supposed to be expected to be educated about their injury, unless something like your book came out, by the way everybody should pick the book up, I will put a link in the show notes.
– [Dr Stuart McGill]Can I say something about that Sebastian?
– [Dr Sebastian Gonzales] Sure.
– [Dr Stuart McGill]We know each other well enough for the last 15 minutes that I can call you Sebastian and you can call me Stuart, how’s that?
– [Dr Sebastian Gonzales] Sounds good, I’m going to get one last Doctor McGill and, okay, everyone Doctor McGill.
– [Dr Stuart McGill]Now I got sidetracked with what I was going to say.
– [Dr Sebastian Gonzales] Myth busting, public education.
– [Dr Stuart McGill]Oh yes, it’s so interesting that when I speak with patients, it’s amazing how often they will say thank you, you’re the first doc who didn’t treat me like a five-year-old, you explained it in a way that we understood, a car mechanic, a plumber, an electrician, a stay at home mom who has to pick out her baby from the crib at 2 o’clock in the morning, they know what a reaching load is, they know the price they pay and the pain pattern afterwards, they aren’t so unteachable, they are in fact easier to teach than some of the high-level docs, they certainly have a longer attention span, I’ll say that
– [Dr Sebastian Gonzales] You mean we have lost already a strong majority of the docs five minutes into this podcast, didn’t we?
– [Dr Stuart McGill]Look, all I’m doing is combating this attitude of medics, that people aren’t smart enough to understand good explanations, I think it’s just that the explanations have been poor, they’ve been purely coached in movement, I lay the fault at the feet of the clinicians, I’m sorry but that’s my opinion.
– [Dr Sebastian Gonzales] Yes, I do agree with that, I mentioned that a couple of times on this podcast before, so I put out some videos on exercise rehab, and I want people to have at least a basic knowledge in it, and I have a good friend who is a clinician who says that we can’t expect people to know any movements through video, we have to cue them, I said I know, but maybe we just haven’t found a good way to do it, I think people are really teachable, it just takes a little bit of time, that’s my personal opinion on.
– [Dr Stuart McGill]My opinion is the same, only stronger, I think great clinicians are great teachers, and again if a person isn’t getting it, I look at the inadequacy of the teacher, have they even considered the learning style, adjust your learning style, think of the patients listening to this, think of the times they’ve been to the doc and they look over the top of the doc’s head, the doc can’t even look up at them and relate to them, and understand whether they’re getting the point or not, or what the progression should be, it’s anyway.
– [Dr Sebastian Gonzales] So you brought up a tangent I should probably take, and we mentioned about short exams, but we haven’t really mentioned the people that only look at MRIs, because there is docs that only look at MRIs and see the structure as the pain generated for these people, can you elaborate a little bit about MRI findings and pain mechanism with back pain?
– [Dr Stuart McGill]Yes, absolutely, first of all this will be heresy to say, but I don’t think radiologists who never see the patient should be giving an opinion on a back image, and I say that for a few reasons, first of all the image shows a picture of the anatomy which shows both the wound and the scar, so what I mean by that is say the clinicians saw an end plate fracture, which is the beginning quite often of a flattening disc, and a broad-based disc bulge, Was that one week old, is it a wound and painful, or is it 15 years old, a scar that is no longer a pain generator, so without having the patient to provide context, as to whether or not they’re seeing the wound or the scar, they shouldn’t be reporting on whether this is clinically significant or not, every single spine you look at you will find issues with it, but they are only interpretable within the context of whatever the patient has shown you as being the clinical causes of their pain, so that’s my first point, there are many clinicians and scientists who argue over the point, well MRI findings aren’t related to pain, and they often bring up the issue, disc bulges, half of people who never have back pain showed disc bulges on MRI and quite the opposite, yes I get that, but if the person has a disc bulge, and the radiologist is on their game, and they really bring up the resolution, and play with the image so they see the nature of that disc bulge, some have an open fissure, delaminated collagen, a direct pathway for the pressurized nucleus in the middle of the disc to seep its way through the delaminations to create what we call a dynamic disc bulge, now clinically that should change shape, if a person sits for a while, or does gardening, or poor form deadlifts, they will pressurize the nucleus, and that bulge will physically grow, so will their symptoms, they will think gardening, sitting in bed lifting very deep causes my leg pain and my back pain, however if I go for a walk, or I preserve in neutral spine while sitting or lifting, I don’t get the pain or the radiating symptoms, so now given that clinical report, and history, the doctor can link whether or not a disc bulge links to the symptoms, but this discussion that MRIs are useless because they may or may not show a bulge, and it may or may not be symptomatic, I don’t think those people have been schooled well enough to know, that you have to have the person in front of you to give that context, now if you have that that scan is very important, because it shows you the mechanism, and therefore you have clues to start trying to see if you can try and wind their pain down.
– [Dr Sebastian Gonzales] So with things like disc bulges, I have patients come in, actually I had a guy yesterday, he was very, I wouldn’t say blaming the disc bulge, but he just couldn’t let go of the idea, and I said how big is it, because he had one two or three years ago, he said three millimeter, and I said I have a three millimeter, we’re very different, we feel very different, so I guess my question is, do you feel we have to get rid of a disc bulge to decrease pain, or does it ever go away, because it seems like a lot of people hang on to the idea that a part of them is broken.
– [Dr Stuart McGill]Well, I certainly know where you’re coming from on that, and there is no answer to the question that you’ve just posed, because it may with one person and not the next, there are some people who show very discalgenic pain patterns, and they have very tiny disc bulges, others have enormous bulges visible compression of lateral nerve roots in the central cord, and they have no symptoms at all, but the ones who do have symptoms are the ones that I’m concerned about, but I never look at an MRI scan or a picture until the very end of the console, or at least until the very end of the pain provocation testing, I want to know what is symptomatic, let’s say we get them to sit on a chair, and they slouch in the chair and pull up on the seat pan so they are compressing their back with a fully flexed spine, and of the person says you know my pain is really ramping up now, all right, let’s lay prone, and I’m just going to apply a little bit of traction to your back for about one minute, now get off the table and stand up, are you better or are you worse, and if they say you know my pain is now gone, what you’re showing is that the disc bulge is dynamic, and if you take a picture of it, and I’ve done this a few times with my radiology colleagues, we will put someone, usually a radiologist with a known active disc bulge into the scanner, but before we put them in, we flex them, and hold them there for 10 minutes, then we take a picture, and the bulge is visibly large, it’s not a three millimeter bulge anymore, it’s a six millimeter, and then we get them to come out and lay prone for five minutes, go back into the scanner, now the disc bulges only two millimeters, so we’ve got an understanding now it’s a dynamic bulge, we can clearly see the open fissure on the MRI, if you know what you’re looking for, now you’ve got a very precise understanding of the mechanism, so if that person can avoid the full flexion that will hydraulically increase the pressure through the fissure and cause the disc bulge to grow, they’ve already found a strategy to manage it, and we have got players in professional sports, all of the professional sports, Olympic athletes, PGA golfers, et cetera, who all have the bulges as I’ve just described, every single one of the ones I’ve mentioned are able to manage it, to some clinical levels and play professional sport, now obviously there are failures in there as well, but there is a guess an answer to the question.
– [Dr Sebastian Gonzales] I think you would be kind of fun to play with the disc on an MRI, I was kind of jealous, so with that being said, since you flex them forward, and I know were only really focusing on disc stuff right now, I feel like flexion, sometimes in the patient’s eyes, I guess to break that down further, flexion would be rounding, rounding forward, or sitting posture, should it be avoided, I’ve seen patients who think that flexion is completely evil and they can’t do it whatsoever, is there a time and place for it, or should it be avoided forever if you have a disc injury?
– [Dr Stuart McGill]Well yes, you’re being very absolute now in the comments, and I know where they’re coming from.
– [Dr Sebastian Gonzales] I’m acting like I’m a patient right now.
– [Dr Stuart McGill]Yes, you’re very good at your interviewing lessons. This is good, well you know again my answer is it depends, what you do is you show the patient the mechanism of their pain, so have them sit on a chair and pull up, but have them sit very tall, and ask them did that cause pain or not, and most of the time if they have a discogenic disc bulge category of pain, they will say you know that doesn’t cause any pain at all it’s very tolerable, and then you say okay now sit slouched, and some of them will say oh yes, when there’s my pain, and I said well now you have a choice, so if you didn’t pull up it doesn’t cause pain okay, you can move your spine and tie your shoes and all these kinds of things, but as soon as you load that flexion, you see that your pain generator, now the curious thing about back pain is it you don’t get used to it generally speaking, if you create pain, you lower the threshold for triggering it again, in other words you sensitize it or tenderize it, but if you can avoid pain, the pain slowly winds down usually, and if you avoid it for a while, the trigger threshold increases, so now you can start have fun, you can go to the dance on Friday night, and move your spine around and have all kinds of fun, it’s not being loaded, but you are moving your spine pain free, but you had to earn that pain-free capacity by avoiding the pain trigger for a while, again, the answer was it depends, if you’re picking up a heavy load, and you flex and cause the pressure through the open fissure, if you have that category of pain mechanism, then guess what, the next day you have a good chance of being locked up again, and having another acute episode, I mean these things don’t come out of thin air, there is a definite mechanical cause, that once it’s discovered and precisely understood, the avoidance strategy again becomes very precise, I mean I can give you examples of, I’ve measured some of the celebrity yoga masters, who contort their spines into all kinds of positions, now if you take a thin branch and bend it around, like a willow branch, it really doesn’t create any stress, just like a thin spine person, who really works on mobility, but what you’ll find is most of those people, the great majority have very little strength, they even have trouble squatting their bodyweight some of them, so if you then contrast that with someone who is the construction worker, or they want to do some powerlifting or dead lift, you have to adapt the spine precisely the opposite way, much less mobility, stiffen up the collagen in the discs to allow the spine to bear a lot of compressive load, generally that favors thicker bone people, if you take a thicker branch and bend it around, it breaks much sooner, because the stress in a round tube is a direct function of its diameter, bigger diameter creates much higher stress when you bend it, so these are all examples of once again the precise, understanding of their pain mechanism lead you to the answer every single time, but it’s not the same answer in everybody, and this idea that people are fearful of moving, I get those patients as well, and almost all the time they’ve been created by clinicians, clinicians who didn’t know how to coach movement, didn’t know how to teach them how to tie their shoe, or sneeze, or get on and off the toilet, in ways that avoided their particular pain trigger, if you have a certain type of arthritis, cystinotic spine, bending forward as you know is a relieving position, or say they have vascular congestion, as part of their back pain and sciatica mechanism, sitting in flexion is what relieves them. So anyway, do you see how again, people try to box me in and commit me to say it’s heresy, never flex your spine, will first of all, do you want to be a yoga master or do you want to set a powerlifting record, but you can’t have it both ways, you know we measured Middle Eastern belly dancers, which was kind of a fun study, I forget how many women we had, but they had amazing motor control, and fantastic ability to move their rib cage separate from their hips, and it was a really fun study to conduct, but you know not one of those women could do a competent situp, and my point was they had this marvelous mobility, but no strength, of course you’re going to find the very rare freak of nature touched by the hand of God who can do everything with resilience, but that’s not the vast majority of people, you have to choose, and once you make that deal be consistent in the training, and you will increase your whatever goal it is, whether you want strength and load bearing or mobility, and do it in an resilient way.
– [Dr Sebastian Gonzales] Yes I listen to a podcast you did, I think it was in Stem, S-T-E-M podcast, and I don’t mean to misquote you if this is not what you said, I thought it was something around different spines for different purposes, is that kind of summing up what you’re talking about?
– [Dr Stuart McGill]Absolutely, have you ever worked with the world champion power lifter, and watch them walk from behind, they have a very stiff spine, and they have to, that’s the only spine will bear picking up half a ton of load off the ground. Now, I know that there are strength and conditioning coaches who were training NFL football players like they were powerlifters, do you know one power lifter that can tie his own shoe, or raise their arms over their head, it’s very difficult to do, so why would you do that with someone who needs to throw a football, which is a very elastic athlete, so a tennis player, or an athlete who has to move explosively, needs a certain amount of elasticity in their body, so these are all examples of tuning the body, and choosing appropriate exercises, which is again, it’s very precise, it’s a continuum, there’s not a yoga master and there’s not a power master, there’s somewhere in between that people can see, but with the right guidance they should be able to find that sweet spot so to speak of maximal function and minimum pain for their body type, and age and injury history and all the rest of.
– [Dr Sebastian Gonzales] Okay sounds good, I think that was the perfect answer, I was trying to box you in last.
– [Dr Stuart McGill]I get used to that.
– [Dr Sebastian Gonzales] I’ve actually been accused by a couple of my friends and people who know me really well, they’re like why do you always ask people questions that leads people down the same path, I’m like I’m really not trying to, I don’t want to lead the conversation, I try to be open ended. So let’s go through some common approaches for treating back pain, because I know a lot of listeners have probably tried this stuff, or they’ve heard it worked for one of their friends or so on, so I thought the first we should hit is rest or avoidance of activity, do you have any input on that?
– [Dr Stuart McGill]Well I’m assuming you’re going to give me a list of these in turn, And pretty much the answer for every single one that I’m anticipating you’re going to answer is, it depends, so that’s why if you follow the algorithm that I put in Back Mechanic, do the assessment, eliminate the cause, and then build the foundation for pain-free movement, so rest and avoidance of activity, well you’ve had patients who are absolutely locked up, they are in excruciating pain, I would say for someone like that, there’s nothing else they can do, but to rest and take it easy that day, they physically cannot tolerate anything else, so for them a very short period of rest, it may last a couple of days, and avoidance of activity, if let’s say reaching their arms over their head to change a lightbulb or something like that triggers a back pain attack, I would say don’t do that for a while, so there are examples, but as a general answer I would say no, you don’t rest and avoid activity, you avoid the activity that triggers the pain mechanism.
– [Dr Sebastian Gonzales] Okay, I like that, I like that. So the next one is going to be, there seems to be a strong movement of people wanting to stretch in lumbar spine, low back for everybody who is listening, how do you feel about that?
– [Dr Stuart McGill]I have strong opinions about that, because I am getting patients caused by it. So I am not the scientist who can pull up our studies who say foam rolling is good or bad for the quadriceps, the deltoids, latissimus dorsi, I don’t have an opinion on that, but I absolutely have an opinion when it comes to foam rolling up and down the lumbar spine, typically a person is lying on their back rolling a foam roller roller up and down, it may be a lacrosse ball or something even more pointed, when you put all your body weight on the spinous process, so that’s the little bone that you feel as you run the thumb up the midline of your back, when you put your full body weight, which puts a shear load on the spine, that is how to create back pain, so now let’s go back one level, why are you doing it in the first place, if it feels good to put pressure on the muscles, I do not think there is a substitute for an intelligent hand, go to a therapist skilled in manual therapy, and get the precision therapy to the location that needs it, but don’t push on the spinous processes with full body weight, that will cause issues, so summary, I don’t have an opinion on other areas of the body, I would not foam roll their low back.
– [Dr Sebastian Gonzales] Okay good, the next one then, I think I’ve heard you speak about this before, if the hamstrings feel tight, should you stretch those if you have low back pain?
– [Dr Stuart McGill]What the answer is again it depends, people who again are in the magical discogenic age group, so let’s say mid 20s, to early 50s, and they perceive they have tight hamstrings when they get back pain, when we measure the source of that, more than half the time it’s not tight hamstrings, its tight nerves, tight sciatic nerves, because of the disc bulge, so get it assessed, and know whether it is because you have a tight nerve, or a tight muscle, now a quick test for your people would be to sit slouched, and if that causes the perception of hamstring pain or tightness, now flex your neck and look down, and if that tightens the hamstring, you never changed your hip or your knee, what you did was change the nerve tension, if that tightens up the hamstring, you’ve got nerve tension, not muscle tension, when you stretch a nerve you will sensitize it so it triggers off in an even lower threshold next time, so absolutely do not stretch that category of hamstring tightness perception, now we can go to the other end of the spectrum where people do have tight hamstrings, and they are stressing their spine because of it, so then it would make good sense to mobilize those muscles.
– [Dr Sebastian Gonzales] I think I was reading your Back Mechanics, it was something to the degree of you were talking about asymmetry with the hamstring?
– [Dr Stuart McGill]Yes, okay let’s talk about that, it’s interesting that in studies of the military, there’s been one in the US, there’s been one in Norway, where they measured the hamstring flexibility of all of the recruits, and who developed back pain over I think the next two years of mandatory service, there really was not a link became coming in with tight hamstrings and developing back pain, however, there was a mild link between having asymmetry right and left sides in hamstring tightness and developing back pain over the next two years, but you know I’m going to say something else, because I’m a Canadian, you’re an American, I’m assuming this is going to be podcast in the US, and the training mentality, the overwhelming training mentality in the US is to lengthen the hamstrings, as if this is good for athletic performance, let me ask a few provocative questions, do you think some of the best dunkers in the NBA have loose hamstrings or tight hamstrings?
– [Dr Sebastian Gonzales] I’m pretty sure are probably tight.
– [Dr Stuart McGill]Absolutely, and I’m the guy who’s measured them, they bounce off a pre-tightened spring, they don’t do a deep squat, they create a spring by pre-tensing the muscle, so they just pop off into the ground after taking two steps to dunk a basketball. We measured the, fella who was the halftime show at the NBA All-Star game, this last time around, the Raptors hosted it it was in Toronto, and this fellow came out, and he is quite modest in height, he’s about six foot one, but he put on the most amazing dunking show, and the NBA players all know this fella, well when you measure his hamstrings, they are tight, tight, tight, he is a tuned spring, when you measure Olympic high jumpers, they have tuned springs, in other words they are elastic athletes, so when you get into throwers, kickers, jumpers, leapers, they are highly tuned elastic athletes, and my advice is be very judicious in how you might want to stretch that hamstring, so there is yet another element for consideration in this whole hamstring stretching question.
– [Dr Sebastian Gonzales] Okay, next one would be, and I do get a lot of people who come in with this, they say that when they cracked their back, their low back, it feels good, so they’re doing it on their own, but sometimes the ask me as well, do you have any input on cracking?
– [Dr Stuart McGill]Well I do, yes, and sorry, it depends, when I see a person, we are starting out the assessment now with an interview, and the interview it might last 20 minutes, or even 30 minutes long, and I’m just listening to them tell their story why they have pain, how they perceive it, and they might do two or three self manipulations during those 20 minutes, now I have a hypothesis, and my hypothesis is they have a proprioceptive that gives very high priority to the stretch reflex, so then I’ll ask them, could you tell me about your current training program, Dollars to doughnuts they’re going to start out talking about mobility, well yes I stretch my hamstrings, and then I do the runner stretch, and do this stretch, and do the scorpion stretch, stretch, stretch, stretch, and I could have predicted that, because that’s the body type and then neurology which likes that behavior, but interestingly enough the most normal response to the stretch reflex is to decrease the joint angle, because it’s a warning system telling your body that is a compromised joint position, one that is now becoming unstable, you probably don’t want to spend too much more time there, isn’t that interesting? And then I’ll say well I pull my knees to my chest in the morning, why, their neurology gives them their jolly, they get 20 minutes of analgesia for pulling their knees to their chest, but what they didn’t realize was, they were being fooled, their proprioception of system gives them the 20 minutes relief, and then the back pain grumpiness comes back in another 20 minutes, so what do they do, they self manipulate and they do another self stretch. And what I say is let’s, now we’ve recognized that phenotype of numerology, every time you feel the need to self manipulate or pull your knees to your chest, I want you to try something else now, and we might defy their mechanism of pain, let’s say it’s a disc bulge, I’ll say now I simply want you to lay on your tummy for three minutes, every time you feel that urge, and is a hard thing for them to do, but after two or three days, they’ll say, do you know what, for the first time I’m winding down my pain sensitivity, and they don’t have the need to self manipulate any more, so there’s just a story that some people will relate to, but generally the self crackers don’t get better.
– [Dr Sebastian Gonzales] Yes, I’ve noticed a lot of things that people come in kind of doing to decrease their pain a lot of it is, I guess not all of it is short lived, I guess it does depend how use that one, but I would imagine they are drawn to that because it just makes them feel good for X amount of time, is there a time and place for things like that, or is it always just kind of the neurology is tricking you?
– [Dr Stuart McGill]You know Sebastian, I don’t really know the answer to that, I don’t know, I am again one of the few in the world who is measured The mechanics and neurological change from some of the chiropractic and osteopathic manipulations, and what we have measured is much more of the neurological change or reset than a mechanical reset, so again it comes back to this idea of neurology and are they manipulating neurology for the better or worse, in terms of pain sensitivity. But once again I think the assessment that understands and probes why they behave and move the way they do, will reveal the pain mechanism, and if it’s part of the mechanism, if they keep self manipulating and they can continue to stay in pain, it’s not working well is it?
– [Dr Sebastian Gonzales] Actually I was listening, I was really intrigued, here’s another reason I wanted you to come on, there was a podcast you were on where you were talking about the fireside evaluation, you have the fireplace set up in the room, and you listen to them and you’re interacting with them, before you even start the evaluation right, it’s just the observation, is amazing to figure out how to manage these people and how to get them out of pain.
– [Dr Stuart McGill]Yes, they come in through the front door, and if I get a chance, I watch them walk out the driveway, and then they come in the front door, and it’s funny you know, if they’re from the southern US, they never ask, they just walk right in, they don’t take their shoes off. But if they’re Canadian, or from the northern US, they will automatically take their shoes off, or they will say shall I take my shoes off? And that is always a huge part of the examination, they revealed to me right away why they have back pain, it’s so interesting that the ones who have flexion intolerance go into full flexion to take their shoes off, usually, not always, but the vast majority of the time, and then they sit down on a couch that we custom-made, it’s very very hard foam, and they mostly sit in their pain, so the extension intolerant back pain person sits in jacked extension, and the person who has a disc bulge generally speaking sits in flexion, and then I have a little pneumatic cushion on that chair, and then I say look, let’s adjust this, and I’ll adjust it opposite to what sitting, and they will usually say, oh, how did you know, that feel so much better, but then they come in and just complete the visual picture, there’s a fireplace, a gas fireplace, and we sit in front of that, and I take a certain body position, it’s at 45 degrees to them, so I’m not in their face, but nor do they ever see the top of my head, which some of them are used to seeing from your usual clinical interactions, I mean the seating is laid out, the lighting, the fireplace, it’s all been well thought out, and then my first question is tell me why you’re here, tell me your story, and I listen to what they put priorities on, is it their job, is that their inadequacy with their spouse, is that their are failing as a parent, to play with their kids, so I’m learning what do we need to do, or they might say something like what have you done in the past, well this last doc told me to exercise and walk and whatnot, but in my neighborhood I can’t go out and walk at night, so for the first time I’m the one that understands that they have a social impediment, they live in a neighborhood where is dangerous for them to walk out at night, so guess what, the compliance will be if I give them exercise in that same neighborhood to go out for a walk in the evening, it’s not possible, there are going to fail. So do you see why, if I’m going to be the guy who makes the difference, I have to understand all of this and put it together to create the best possible plan, these are people, I don’t see the average back pain patient, I see the one whose failed 10 different approaches, and that they are at the end of their wits now.
– [Dr Sebastian Gonzales] I think it’s amazing the time that you spend, and we definitely don’t spend as much time here, I try to at least spend an hour the first time, and I always tell them that we might not get to any hands-on, we might not get to anything, we might get to only just assessment, but it really depends on how far the rabbit hole is you know, but I think it’s important to go the right direction, rather than just speed off in the wrong direction, something I think you should definitely speak about on here is building a resilient back, and I know you have the McGill big three exercises, and I know that correlates with the core and how it works and so on, can you go a little bit into proper core training and the big three?
– [Dr Stuart McGill]Yes, if I could just pre-face that Sebastian, I know I’m known for the big three, but we do so much more than that, and there are some people that think those are just the McGill exercises and that’s all he does, that will not get people into the Olympics, and into the UFC and all that sort of stuff, of course this is just the beginning, but what is required to build a pain-free foundation, is a strategic tuning of the body, so we’ve talked about elasticity a little bit and mobility in the head and shoulders, but core stability is nonnegotiable for pain-free function for three main reasons, and I give the three reasons now, and I should also say that there are very few university laboratories in the world that measure spine stability, that means everyone else is just hand waving about it, they’ll say oh that’s a stable pattern, but how do they know, how do they know what the muscles are that actually create a stable spine, well as I said we were one of the institutions that quantified stability and measured it, so with that preface, the three reasons why core stability is nonnegotiable, are these, the first one, the spine by nature is a flexible rod, well it’s nice to have a flexible rod if you want to dance, or if you want to throw a ball, or tie your shoe, very handy, but in all of those times when you’re moving your spine around a lot, if you put high load on it that increases the risk of mechanical damage, so when you’re picking up something heavy, and it might be a stay at home mom picking up her baby 2 o’clock in the morning, or it might be a office worker who wants to come home and do a little powerlifting, they have to stiffen that flexible rod to allow the flexible rod to bear load, they’ve got to turn it into a beam, so you do that by strategically bracing the core muscles to stiffen the rod, and that unleashes the hips to be ball and socket joints and you hip hinge and all the rest of it to create this very resilient linkage, the second reason has to do with proximal stiffness for distal athleticism, so let me start off with an example of a pec muscle, so your bench press or chest muscle on the proximal side of the shoulder connects to your rib cage, on the distal side it connects to your arm bone or humorous, when you activate that muscle it flexes your arm around on the distal side but on the proximal side it bends your rib cage towards your shoulder joint, so if all you used was the bench press muscle to push somebody or push an object you would collapse, your torso would rotate, your rib cage would bend towards your shoulder joint on the proximal side, and it would mildly pull your arm around on the distal side, but if you could lock down your core so 100 percent of that muscle contraction was sent to the distal side, your arm would come around with great force, so do you see why you had to stiffen approximately to get distal mobility, just like a tractor has to put down stabilizers to anchor into the ground to allow the bucket to actually dig the earth, if you don’t put down stabilizers the whole tractor just moves around. So now let’s talk about walking, in order to walk you have to stand on one leg and swing the other through, if you don’t have core stability, your pelvis drops down on the swing leg side. If you go to the neurology ward of the local children’s hospital, you might find a child with a paralyzed quadratus laborum, that’s a core muscle, a very important core muscle that runs up and down either side of the spine, when they take a step, so say their left QL is paralyzed, when they stand on the right leg and swing the left leg double pelvis collapses and falls down on the left-hand side, you need those core muscles to hold your pelvis up to allow the legs to drive you forward, otherwise your torso just bends and the spine collapses, so this notion of proximal stability is absolutely critical, there’s no linkage in engineering that could function otherwise, now the trick is to tune that stability and stiffness, so if all you’re doing is bending down to pick a pen that you dropped on the floor, you need mild stiffness, but if you’re going to pick half a ton off the ground you need a lot of stiffness, so that’s the tuning aspect that people don’t often get, some people coach it poorly and over brace their patients, which I think you alluded to earlier, that the person is way too stiff and there just crushing themselves. The third element to core stability are joint micro-movements, so let’s use a knee injury example, consider a knee where the ligaments have been partially torn or stretched, the doc performs a drawer test, in other words they shear the knee, and see micro-movements that indicate the integrity of the knee, and if it’s pain generating it sends off a flash of pain to the patient, well we do exactly the same thing with spines, if a person has disrupted a disc or the ligaments, that particular joint becomes a bit lax, but when you probe that with your thumb, you will find which joint has micro-movements which are causing pain, then ask the person here let’s try this abdominal bracing strategy, push your fingers into their abdominal wall laterally, and say push my fingers out, and then probe the painful joint, and if they say oh you know that doesn’t cause me any pain, you just proved that it was the micro-movement and laxity that triggered their pain, but you have just found a bracing strategy to take their pain away, but the patient might also say, oh no, that bracing causes more pain, all right they have compressive intolerance then you might say let’s try a pec/lat compression strategy and see of that works, so in other words we play with the bracing strategy to control the pain causing joint micro-movements, anyway there are three quantitative and measurable explanations of why core stability and core athleticism and tuning is nonnegotiable.
– [Dr Sebastian Gonzales] Okay so when people choose their core programs, I know probably a lot of people are on the other end thinking I’m going to go pick some stuff off of YouTube right now, is there are criteria that they should be looking for when they choose an exercise for the core or do you have some suggestions on that?
– [Dr Stuart McGill]Man, you’re good at your job. Yeah well that’s how we came up with the big three, so let’s take someone at the low end of the clinical spectrum, they have diagnosed now a little bit of instability, as a part of their pain mechanism, so how do you get them going, we came up with the big three, we didn’t invent those exercises but we quantified a broad spectrum of stabilization exercises where we try to minimize the load on the spine, so you have to spare the spine, otherwise the exercise will just create more pain, but you have to guarantee that you’re actually stiffening and stabilizing the pain mechanism, so those were the three exercises that kept bubbling up to the top of sparing the spine and guaranteeing stability, so that’s where they came from, but of course Back Mechanic really gets, it’s whole point is to get people out of pain, but it doesn’t train them, so then we move them to my second book Ultimate Back Fitness, and we shift the paradigm, they are out of pain, but they have a history of pain, we won’t go back and trigger the original offending instigators, but now they have to judiciously create a progressive program, they may incorporate the big three, but then we would add more stabilization work for sure, but again your listeners might find this interesting, there’s one category of back pain patient that right after doing the big three exercises they’re pain free, and they’re pain free for a couple of hours, and what we measured with that subcategory is, they have a residual stiffness, their new neurology after doing those exercises keeps a tone to their core for an hour or two afterwards, we find that some sprinters sprint faster, they get to cut a little bit harder because proximal stiffness is greater so that muscle activation is creating more athleticism distal to the hip joints and shoulder joints propelling the arms and the legs, so again there is wheels within wheels, as you know my never ending source of fascination and entertainment and everything else for the past 32 years.
– [Dr Sebastian Gonzales] Yeah, with those people, you said there is a subcategory then, because everybody on the other end is probably thinking I wonder if I’m not one, I wonder if my back pain could be lucky enough to where it feels good after these exercises, what type of symptom patterns do those people have, or have you recognized anything that they have in common?
– [Dr Stuart McGill]Oh what a beautiful question, you know, we have got to syndicate you, you are good at this. Well yes the answer is, what I would ask people to do is establish a baseline, so stand up and know your pain, so know its location its pattern and its intensity, now do the big three, don’t do major reps and sets, maybe do three 10 second holds, another three 10 seconds, and then another three 10 seconds, and then stand back up again, if the patient now recalls their previous baseline, they will know if they are better or worse, if they just got better, beautiful, we just found a replacement activity that gives them some temporary resilience, what we would say to that category of patient is you’re going to do your big three twice a day, do them mid-morning and mid-afternoon, now we’re creating two windows of opportunity, it’s like giving them a drug or an opioid, only there’s no side effect, so slowly we’re winding down their pain sensitivity, and creating a bigger window every time.
– [Dr Sebastian Gonzales] Okay, I guess my question further on that note is, if the stand up and there on pain medication or some type of thing that numbs the pain, they can’t assess it right?
– [Dr Stuart McGill]It’s better not to be on pain med is of course, any time you’re registering pain, so one of the instructions to any patient coming to see me, is try and not take your pain meds on the day of the consultation. So I’m getting a very true read of therapy and sensitivity.
– [Dr Sebastian Gonzales] Okay, so you mentioned holding for 10 seconds, and I saw you put some stuff out there before on endurance versus strength, the terms at least in regards to core, why do you suggest 10 second holds, because I know people do glorification of holding planks for 10 minutes now.
– [Dr Stuart McGill]Will that’s not to get people out of pain, that’s to show off to your friends, or it’s for performance training whatever it happens to be, but that is not a strategy to get out of back pain for several reasons, the first reason, why 10 second holds, well you’ll find that some people get back pain because of muscular ache, when you do the big three, virtually any isometric exercise, the muscle contracts and goes into a turner that clamps down the capillary bed, so the internal blood supply of the muscle is shut off, once you go into an isometric contraction like that, so that will create back muscle cramps in some patients, but what we found, we measured with near infrared spectroscopy, which is instrumentation that measures blood oxygenation and muscle, hemoglobin and myoglobin in the muscle, and it starts to drop off rapidly in oxygenation after about eight seconds, so that’s why we release the muscle every 8 to 10 seconds to reperfuse with oxygen and minimize the chance of back muscle cramps in an already back pained person, the next reason why we need to build endurance before strength, is the majority of current back pain people have back pain because of the way they move once they get tired, think of the last time you hurt your back, or tweaked a painful body part, it’s when you broke form, so we measured this and proved it in autoworkers and Hydro alignment, guys who climb hydro poles, we measured guys chroming Chrysler car bumpers, which weigh about 75 pounds, do you think it was the strong ones or the moderately strong ones that got more instances of repeated back pain throughout the year?
– [Dr Sebastian Gonzales] It was probably the strong ones wasn’t it?
– [Dr Stuart McGill]It was the strong ones because, they would lift the car bumpers no problem for a few reps, but then they get tired faster, and when they get tired they broke form, and that’s when they hurt their back, but the other guys who were a strong but had more endurance, could lift with perfect form to protect their back and joints for many more repetitions throughout the day, so there’s a little bit of nuance to that being strong or durable, it’s the ratio, if you have a lot of strength and your work and you do different jobs, then you need a foundation of endurance to keep good form, if you’re an Olympic weightlifter, and you come out and do one world-record Olympic lift, that’s one exertion, you don’t get tired, and there’s not a second rep to break form on, so it doesn’t matter, but now think of some of these exercise programs that you might be familiar with, where first of all the athlete does 10 burpees, and then they go do 10 Olympic lifts, and when you look at the 10th Olympic lift, it’s horrible form, now you know why you’re seeing them as a patient, they broke form because of the programming, so I don’t know Olympic lifters that do 10 repetitions, they might do a single lift or a double or a triple at the most, at least the ones I work with, I worked with some pretty good ones, but they never ever train to fatigue, but that’s when you get hurt when you’re handling high loads, so that’s why the insurance foundation is so important for people who are exerting high strength repeatedly. So there’s some nuances in there as to why endurance is important, another one just came to mind, so you know that there are certain patterns of movement that back pained patients need to follow to avoid their particular pain triggers, well sometimes if a little bracing makes them more resilient and takes the pain away when their gardening, okay, they learn to do that, that’s not a strength challenge, that’s an endurance challenge once again, so the way out of back pain is not in strengthening the back, in design of the program, it’s by designing an endurance back program, and of course they get stronger as a side-effect, but that’s not what is programmed.
– [Dr Sebastian Gonzales] Okay Stuart, I’ve got a good one to follow up on this. I’m going to quote what a lot of people say to me, I have a weak low back, can something like that address issues were people have weak low backs?
– [Dr Stuart McGill]Well look, it depends, if that doesn’t surprise you. When a person comes and says I have a weak low back as an excuse, then I will try to detect that, and I will try to figure out a way how can I empower this person, I’m not going to tell them, your weak and you’re weak minded and all the rest of it, no, I’m going to detect that they probably have a lack of confidence, because the experts have told them to do things in the past that have only hurt them, so all they have known is failure, I have to figure out a way to empower them, and it’s usually proving to them that I can take the pain away, so I will create their pain, I’ll say to them, show me what causes your pain, and then immediately if I can define the pain mechanism, I will try to mitigate it somehow and show them you just tuck your pain away, now that may involve a little bit of strength, and I’ll quote my good friend powerful Pavel Sasoli, strength is a skill, and when you show a person how to use their body, all of a sudden they unleash what strength they had, but they didn’t know how to unleash it. So I have a weak back, figure out the way they can start moving and training in a way that doesn’t trigger their pain and gives them some confidence that they can continue the progression, and get what we would then call sufficient strength, and I’ve measured some of the top athletes in different sports, with the exception of powerlifting, the best players are not the strongest players, obviously in powerlifting the strongest guy usually wins, but in America football, hockey, baseball, UFC, it’s not the strongest two wins, the strongest guy tends to push his punches with muscle, their slow, it’s the elastic fighter who can snap and land with precision who is the deadly UFC fighter, so it’s so interesting, just try and achieve sufficient strength skillfully, and in a resilient way, so figure out why they’re saying I have a weak back, and go with it accordingly.
– [Dr Sebastian Gonzales] I feel like that is a perfect answer to start closing the podcast down, but I can’t let you go until I hear what you personally do for your back, or spinal health?
– [Dr Stuart McGill]Well the answer to that, and I wasn’t anticipating that one at all, very few people ask me that, I don’t know if you’ve ever been to one of my courses, but a, I have to train to be able to put one of those courses on, and if I go and work, I mean I’m putting on a performance enhancement course at Chris Duffin’s Kabuki Strength up in Portland at the end of the month, you know I’ve got to be in shape to do that, I can’t be a skinny old man working in and asking do you mind handing me that kettle bell, it doesn’t work, but I also have quite an injury history myself, and then also I’ll reveal I’m in my 60s, so what I do for my own back has radically evolved over the years, there’s no question, I played football and hockey as a young man, and I played old-timers hockey into my 30s, so I was definitely training for performance then, and I paid for it, I even did a little bodybuilding in my late teens, and then tried for maximum strength in personal bests and all the rest of it, then in my 40s and really into my career as a professor and a clinician, I had to back off on that, I got a bit soft, but I did my core work, the big three, a little bit of hip mobility, shoulder mobility, et cetera, now I train not to lose any more, I don’t want to gain any more, so I do balance training, I do foot work, which living in Canada you have to recover from falls on slippery surfaces, I spent a lot of time in the woods crawling over slippery rocks and logs and that kind of thing, so I have to keep a reasonable amount of mobility, I work on grip strength, and my grippers haven’t declined very much and they come in darn handy, I can also tell you I’ve had hip replacement, so I do a gluteal reprogramming exercise routine every day, a little bit of hamstring and salas lengthening, that’s about all that I can think of at the moment, but it’s certainly been a phase through my life.
– [Dr Sebastian Gonzales] I can’t get past that somewhere out there there’s pictures of your bodybuilding competition.
– [Dr Stuart McGill]I never went into a competition no, I was just interested in American football through high school and university, so I had to keep the beef on, and that was really the way to do it then. I’ll tell you, in those days it didn’t help me to attract women, I’ll admit that
– [Dr Sebastian Gonzales] That didn’t help, I thought you just wore a tank top in the summer in Canada and had the pythons hanging out?
– [Dr Stuart McGill]I’ll tell you that didn’t work for this fellow at all, but I ended up with a pretty good wife though, I don’t know what on earth she found attractive, but anyway.
– [Dr Sebastian Gonzales] You’ll probably be happy to hear I don’t think that works much in America either. So how can everybody reach you, I’m going to put the show notes in the show notes for your Back Mechanic book that everyone should definitely get, how can they reach you if they want to find out more about you and the stuff that you put out?
– [Dr Stuart McGill]Well we do have a website, backfitpro.com, and it’s just as it sounds, B-A-C-K-F-I-T-P-R-O backFitpro.com and it has links to our books and videos, there’s a lot of information on there though, there’s quite a number of free videos, links to some YouTube work, a few articles, yeah I guess that sort of thing, there’s also a list of providers as well, and we don’t take that designation lightly, I refer to our network of providers, I’ve worked with them all, they’ve all taken my courses, and I’ve personally worked with all of them and make sure they are very competent in performing an assessment that will reveal the precise cause of the person’s pain, and they know what to do to coach the person and empower them to desensitize their back issues, and in some cases for the athletes, build that resilience and performance once again.
– [Dr Sebastian Gonzales] Also, is there anything you think we missed on here that anyone needs to know?
– [Dr Stuart McGill]I don’t think so, if this is my last bit, I’m going to say something Sebastian, you are good at your job, I think Joe Rogan better look out, you did a phenomenal job on that.
– [Dr Sebastian Gonzales] Well thanks, I’ll be honest with you, some of the people I interview, I’m a little intimidated, I don’t know if I can do this interview well, so it takes me a little while to listen up, it’s not something that I’m developing overnight, my first podcasts were terrible, so thank you for the praise.
– [Dr Stuart McGill]Well we all wish we could have those back, I was out driving this morning and I drove by the church, and you know how churches have different marquees out front, and the saying this morning struck me, and it said everyone gets a second chance, it’s called tomorrow. Isn’t that beautiful?
– [Dr Sebastian Gonzales] Yes it is, I don’t know who makes those things, but they have good sayings ON those things. Well cool, thank you for coming on, I will put all your contacts and all the links in the show notes, and sounds good, thank you Doctor.
– [Dr Stuart McGill]Yeah fantastic, thanks for all of that, and hope your listeners obtained some value.
– [Dr Sebastian Gonzales] Awesome, all right everyone that was Doctor Stuart McGill, always great on podcasts, I always like to hear his, he does have a lot of information out there and other podcasts, again the reason why I thought I would include this question for you guys, it’s mainly because we still have a lot of patience misunderstand back pain, and even when I referenced some of the other podcasts, which were amazing by the way, they still didn’t understand it, because I think it was a little too technical, so I thought I would go down a questioning series that we get asked a lot of as healthcare providers, I will put this on the website, so it’s P2sportscare.com/podcast is where you can find the show notes, and you can find all of the stuff for Doctor McGill and what he spoke about on the podcast, if you haven’t gone to iTunes are ready, please go to iTunes and subscribe to this, and by the way, I’ve barely found out, I was looking and trying to find out where I can find reviews for myself, or actually reviewing other podcasts, because I’ve been on other podcasts, and I wanted to check theirs out, and also leave one too, and I couldn’t find for the life of me how to review a podcast, so it took a little bit of digging, so if you don’t know how to review the podcast, just go to Google and put in how to review a podcast, and it will take you down the question series, so that’s how you do it, I greatly appreciate any feedback good or bad you have on that, honest feedback, I will speak with you guys soon, if you have more questions or experts that you want on, reach out to me on P2sportscare.com, talk to you soon.
Attention Law Enforcement:
Here’s your Checklist for the Stiffness Workshop