This is the ultimate article to hip impingement (AKA femoroacetabular impingement) in 2021.
In this new article I’ll show you:
- 7 Facts About Hip Impingement Your Therapist Didn’t Mention
- Symptoms/ On-set Of Hip Impingement
- Is Hip Impingement Caused By Low Flexibility?
- Why Does Squatting Deep Hurt My Hip?
- Types of Femoroacetabular Impingement
- Does Hip Impingement Require Surgery?
- Stretches and Exercises For Hip Impingement
- …and lots more
Note: read the disclaimer and always see a doctor first. If you need some help virtually (or in-person) the “Locally World Famous Chiropractors®” at Performance Place Sports Care are ready to work with you!
Let’s get started.
What is Hip Impingement?
Hip Impingement is a condition of the hip joint where bony or cartilage structures become painful due to repeated friction. It’s characterized by a loss of hip flexion, internal rotation and adduction. Other names are femoroacetabularimpingement or FAI of the hip. Often times painful with sitting, walking and crossing legs. Many times lower back pain occurs in combination with hip impingement.
I’m Dr. Sebastian Gonzales and I put together this article so you would only have to look in one place for all of the current information on hip impingement. Enjoy the read and contact me with any questions. My references are all at the end of the article.
1: Femoroacetabular Impingement is often slow onset
Often athletes think an injury happens from a single incident or action, but that is rarely the case. A study of the 2012 Olympics in London showed around 70% of all USA team injuries were actually from cumulative trauma, or in other words were “non-traumatic.” This means that no other athletes hit them, they didn’t fall on anything, nor was any “tear” felt during competition.
2: Femoroacetabular Impingement creates compensation
When walking on an injured leg/ hip a limp is created. A limp is a form of a compensatory or “altered” motion. Femoroacetabular Impingement creates changes in the way you move.
For example, if you are a catcher, you will not be able to get into a deep squat (below 90 degrees) without pain, thereby creating a shallower squat or leaning your weight onto the opposite leg.
If you are a pitcher and the painful hip is your lead leg, you will not be able to bring your leg very high during your wind-up. Furthermore, you will be resistant in wanting to put all of your weight onto you lead leg as you land and rotate your body through the follow through, yielding your pitches high and to the glove side.
3: Surgical correction is not a replacement for rehabilitation
Surgery is intended to correct a damaged structure. It is not intended to correct bad habits. It is extremely common for pitchers to create compensatory motions while guarding an injury. Hip injuries will lead to asymmetrical loading of the legs during strength and conditioning and changes in throwing mechanics. These are just a few compensatory patterns.
Generally speaking the longer the pitcher has the injury the more ingrained in poor motion they will be. Rehabilitation of an injury is a physical and mental process.
The physical process will encompass strengthening, stretching, and so on.
The mental process encompasses recognition of compensatory motion and ways to combat them.
Bad habits don’t go away quickly, or easily, hence the reason pitchers have a pitching coach for their entire career.
When surgery is needed, rehab is needed as well. However when rehab is needed, surgery is not always needed.
4: Everything is connected
You remember the song your grandmother used to sing about the “hip bone’s connected to the thigh bone” and so on? It’s all true. But what the song left out was muscles, tendons, fascia, ligaments, and cartilage.
To throw a fastball so many parts of the body need to be functioning at the same time. If even one fails you will have a drop in velocity and compensatory motion, leading to injury. Studies estimate around 51-55% of force through the baseball is supplied by trunk and lower body. Only 13% of the force is supplied by the shoulder.14, 23 That is a massive amount of power to lose if your legs and hips are not functioning well.
Wondering how that force gets from the legs to the arm? Look what’s between the two areas. It’s the trunk. The body is all connected and if stability and motion are not optimized your mph will be lost to your weakest areas.
5: Femoroacetabular Impingement Exercise can help
There are exercises you can do as a pitcher that will help decrease advancement and symptoms of hip impingement. The body is designed to move a certain way. When it does not move in the way that it is intended, pressure/ load can be put on areas that are not designed to take that load.
Every muscle, tendon, bone, ligament and cartilage is designed to tolerate a certain load capacity. When pushed beyond that load, to put it simply, it will break. Exercises for the core, pelvis, and hip can optimize how the body loads its parts.
Here is a short list of some rehab activities that will help a pitcher optimize their hip function:
- Squats
- Deadlifts
- Cleans
- Floor Core Work
- Pallof Presses
- Plyometrics
- Static Stretching
- Dry Needling
- Acupuncture
- more
6: Femoroacetabular Impingement surgery recovery time
It’s a range just like anything else. But, your health before you get wheeled into the operating room is one of the largest predictive measures of how long it will take for your recovery. Well-conditioned, professional athletes can be back around 3 months. Non-active, over-weight individuals can take more than a year.
If you are considering a surgical intervention you should be in the best possible shape before you undergo the surgery. Preparation is possible with correct eating habits, weight control, resistance training in non-painful ranges, stretching and more. Creativity in program design by a Sports Injuries Specialist is critical.
Do not attempt to design it yourself. I have seen many try and fail after months of frustration and flare-ups.
7: The Pelvis is the key to correction
One of the latest studies regarding Femoroacetabular Impingement, said this:
“Rehabilitation for patients with FAI should include attempts to improve dynamic muscular control of the pelvis with resultant changes in pelvic tilt.” 15
Everyone is welcome to dig into that study, but for those of you who don’t understand technical anatomic and biomechanical language, I’ll do my best to break it down.
What is dynamic muscular control?
Simply put, this means controlling your body while in motion, rather than at rest. The external load can be gravity, change of body position, change of direction/ velocity and more. In throwing a baseball, our pitchers are subjected to more than one external load. Now we have to teach them to “feel” where their pelvis needs to be and then how to keep it there while the body position changes during a pitch.
Why do pitchers need to have dynamic muscular control of the pelvis?
So our pitchers can optimize their pelvic tilt. Pelvic tilt is normally assessed as being anterior (forward) or posterior (backwards). Changes in pelvic tilt significantly affect positioning of the socket of the hip joint. This has been validated through imaging studies. 15
Here are the goals with our pitchers:
- Find the correct pelvic tilt
- Mentally be able to find that tilt again,
- Remain in that position when subjected to manual perturbations
- Remain in that position during changes in body position
- Then break down the pitching positions and subject to manual perturbations
- Then increase speed
- Ask the pitcher how they can improve (mentally checking in)
EXPECTATIONS WHEN YOU
COME SEE US IN COSTA MESA:
MORE THAN 50% IMPROVEMENT WITHIN 4-6 SESSIONS
Most Cases
MORE RELIEF WITH LESS RISK
We Only Use High Reward/Low Risk Treatments
NO RIDICULOUS LONG-TERM TREATMENT PLANS
MORE ATTENTION WITH A SKILLED GUIDE
Even Though our Costa Mesa Chiropractor are Not A "Real Doctor" 🙂
MORE THAN A TYPICAL COSTA MESA CHIROPRACTOR
No Bone Cracking Required To Feel Good
NO QUACKERY
Dr. Gonzales & Costantino Only Uses Current Evidence-Informed Methods
CLICK HERE TO BOOK YOUR APPOINTMENT WITH A COSTA MESA CHIROPRACTOR
BOOK AN APPOINTMENT
How Common Is Hip Impingement?
Femoroacetabular Impingement can happen in many different sports and athletes of different genders. Normally it is found in higher correlation with athletic populations in predominately young, white athletes with normal basal metabolic index (BMI). We use to believe it was a condition men would only get but women are not immune from it by any means.1 This is probably because girls take part in more youth sports than now.
CAM deformities have been found to develop in highly active young athletes, more so than non-athletic ones.
Development of a CAM deformity can be correlated with high activity levels where the growth plate of the femur has not totally closed. Typically, athletes will experience lack of the abduction, flexion and rotation from the CAM.
What sports are safe for these CAM athletes?
Logic would lead us to believe that the more we require the athlete to be forced into the pinched motion, the more damage to the joint. This can lead to labral tears and femoroacetabular impingement. The CAM deformity decreases the athlete’s ability to move the hip into flexion, adduction, and internal rotation. Take a look at the motions required by the sport and see if these motions are needed to high degrees.
Some sports you should be aware of are:
- Golf
- Baseball
- Tennis
- Lacrosse
- Gymnastics
- Ballet, and other types of dance

In the past, many clinicians have felt femoroacetabular impingement was idiopathic, or that it arose spontaneously.
Yet studies have continually shown a higher association in athletic populations than in non-athletic populations, which leads us to believe that there are other correlating factors. One study noted around 55% of all patients are female with the typical surgical age of 28. 2,3
A recent systematic review found that there is a higher correlation of CAM deformity in athletes participating in high impact sports (i.e. basketball, hockey and soccer) over non-athletes. 3
A radiology study showed a correlation of CAM deformity development in youth soccer players whose growth plates are still open.
High prevalence of CAM deformities were found via x-ray in these kids even after initial x-rays showed no signs of CAM development two years earlier.
Overhead athletes are especially high risk due to the need of larger energy motions of the hip.
This demand on the hip can lead to labral tears and increase symptoms of CAM deformity.
Logic says our young athletes involved in club sports and year round programs will have a higher potential of CAM deformities than those who take breaks, or change sports.
Hip Injuries in Major League Baseball
Noteworthy players in Major League Baseball with hip injuries:
- Josh Beckett – Femoroacetabular Impingement
- Devin Mesoraco – Femoroacetabular Impingement, possible labral tear
- Alex Rodriquez – Femoroacetabular Impingement from a CAM deformity

Josh Beckett Hip Impingement
With Josh Beckett being a pitcher, there is a large need for a normal functioning hip with normal range of motion, strength, and power.
While analyzing Beckett’s outings where he complained of hip pain, his reports of pain were commonly made during the later innings when his command and control decreased. More pitches went up in the zone to the glove side.
These findings are not uncommon for pitchers that use less legs/ hips in their delivery4. They are depending upon more of the upper body for their velocity. Because of this, pitchers unable to use their legs/hips can, and probably will, develop shoulder injuries, such as rotator cuff tears and SLAP tears.
Do not continue to pitch without knowing how to use your lower body.
You will only experience low velocity, less command, more frustration and more shoulder pain as time goes on. Shoulder injuries in pitchers typically develop from lack of proper deceleration.
Femoroacetabular impingement in pitchers can ultimately lead to lower stride length, and poor command of pitches leaving them high to the glove side.
While pitching, up to 75%-80% of the power and velocity comes from the lower body or the legs. When a pitcher or player is unable to properly transfer a load from the lower body through the trunk and then the shoulders, there is a high possibility of decreased performance and/or a resulting injury.
In cases of hip impingement it is extremely common for hip mobility to decrease. This will affect a pitcher’s ability to attain proper positions in their wind-up.
Devin Mesoraco Hip Impingement
Another major league baseball player who has developed symptoms of impingement, is Devin Mesoraco of the Cincinnati Reds. As of July 18th 2016, he underwent his third hip procedure, this being a season-ending one.
The reason I’m using him as an example is because he’s not a pitcher. The catching crouch position actually requires more hip flexion than a pitcher or any other position in baseball. In a more advanced case, femoroacetabular impingement can become a labral tear, which usually requires surgical correction based upon the type and degree.
Incidence of players requiring hip surgery per season from 2002-2006 was 1.5 players. It rose to 6.5 players from 2007 to 20115.
It is important to realize surgical cases are the most advanced forms of these conditions. Many players with anterior hip pain do not actually report it, leading to more advanced degrees of injury.
Femoroacetabular impingement is more common in sports than you think.
Alex Rodriquez Hip Impingement
Back in 2012, A-Rod (Alex Rodriquez) was the poster boy of hip injuries in the major leagues. He eventually underwent surgery with Dr. Brian Kelly to shave down the over-grown portion of the femoral head and neck.6
Shaving down the femoral head is a correction for CAM deformity.
Remember, CAM deformity develops in younger, highly active players before the growth plates close.
It is a preventable condition but youth activity levels need to be scaled. A-Rod was very fortunate to have down time anyways, for legal reasons, to regain his motion, strength, and coordination of the hip/trunk after his surgery.
As you can see hip injuries in baseball can happen. A majority of the time, they start from a CAM deformity at a young age, leading to femoroacetabular impingement, which can lead to labral tears ending in a surgery/ the DL.
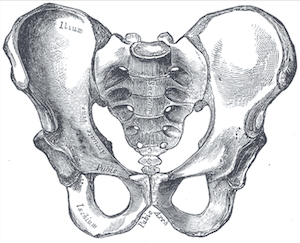
Anatomy of Hip Impingement
To really understand types of femoroacetabular impingement we have to start with hip/ pelvis anatomy. The hip is considered a ball and socket joint, with the ball being the femoral head (top portion of the thigh bone). Three bones called the ilium, the ischium, and the pubic bone form the socket, otherwise known as the acetabulum.
Important anatomical structures surrounding the joint include bones, ligaments, cartilage, muscles and tendons.
Bones of the Hip
- the femur bone
- the ischium bone
- the ilium bone
- the pubic bone
Cartilage of the Hip
As for cartilages, there are two important types in the hip joint.
- Articular Cartilage
- Fibrocartilage
The articular cartilage is located on the ball of the femoral head. The purpose of the articular cartilage is to decrease friction, and create a smooth surface for two bones to slide against each other.
Fibrocartilage makes up the labrum, which is located on the inside portion of the acetabulum (socket). Fibrocartilage, created with a very different substance than articular cartilage, is for a different purpose: the labrum acts similar to a gasket or an O-ring, creating a tight seal for extra stabilization of this already mobile joint.

Ligaments of the Hip
There are three extra-capsular ligaments of the hip attaching the femur to the acetabulum, or, in simple terms, the ball to the socket. Extra capsular ligaments reside outside of the joint.
- the iliofemoral ligament
- the ischiofemoral ligament
- the pubofemoral ligaments
There’s one intra-capsular ligament. Intra-capsular means is inside the joint.
- the ligamentum teres

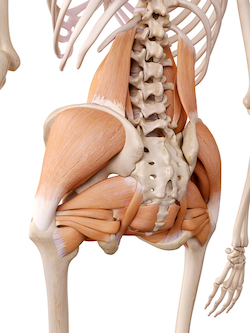
Muscles of the Hip
You should be very familiar with important muscles of the hip and their related tendons.
- the iliopsoas (hip flexor)
- the rectus femoris (hip flexor/ knee extensor)
- the “hamstrings” – semitendonosis, semimembranous, and biceps femoris, long head (hip extensors/ knee flexor)
- the gluteus medius (hip abductor/ lateral hip stabilizer)
- the tensor fascia latae (hip abductor/ flexor)
- the iliotibial (I.T.) band (hip abductor/ lateral hip stabilizer)
- the gluteus maximus (hip extensor/ external rotator)
- the piriformis (hip external rotator)
- the superior and inferior gemellus, obterators, quadratus femoris (hip external rotators)
- the pectineus
- the adductor longus, magnus, brevis (hip adductors)
- the sartorius (hip flexor/ external rotator & knee flexor)
- the gracilis (hip adductor/ knee flexor)

Muscles of the Trunk
Proper function of the trunk, what generically you may call the “core,” is critical to rehabilitation and prevention of femoroacetabular impingement. The general rule is, if you can control the pelvis/ ilium then you can control the hip. Everything is connected, and in cases of hip impingement it is directly connected.
Some muscles of the trunk to know moving forward are:
- the internal oblique
- the external oblique
- the rectus abdominis
- the transverse abdominis
- the quadratus lumborum
- the multifidi
- the paraspinalis
- the lumbosacral fascia
Biomechanics of Hip Impingement
- Flexion – bring the knee towards the chest
- Extension – opposite as flexion
- Internal Rotation – bringing the toes inward, with a straight knee
- External Rotation – bringing the toes outward, with a straight knee
- Adduction – bringing the feet/ knees against each other (toward midline)
- Abduction – opposite of ADDuction or away from midline
Without knowing the basics of hip motions, you will not understand muscle and tendon function. Some of the best educational papers on ball and socket joints, such as the hips, include these types of terms. You must understand these motions or your education should stop here until you commit them to memory.
Symptoms/ On-set Of Hip Impingement
Common symptoms include:
- clicking
- popping
- catching of the hip
- deep inner groin pain
- pain feels “inside” the hip
- pain with sitting for long periods
- pain with driving
- groin pain with sitting on the toilet
- pain with standing up from a seated position
- pain with putting on sock/shoes while seated
- pain while walking stairs
- pain with walking up hill
- slight or large limp
- pain with sitting cross-legged
Symptoms of femoroacetabular impingement can range greatly based upon the degree of the injury. It is not uncommon for athletes to have small symptoms of femoroacetabular impingement for years, and to think it is simply hip flexor tightness.
However, when symptoms are present, no matter how small, it is an indicator of damage occurring to the cartilages of the hip.
A limp will become more noticeable in later stages. These changes in movement patterns or “habits in motion” have been researched extensively. Changes in your movement will lead to altered weight on different joints and muscles of the leg, leading to further injuries. Often times, you may even see pain developing in the opposite hip, knee and foot after a severe limp.
When we take into account the range of motion sitting cross-legged requires, it makes complete sense. The cross-legged position requires flexion, internal rotation, and adduction.
All of these movements in combination with each other will narrow the space in the joint, thereby creating impingement on the structures of the femoral head.
With baseball players, especially pitchers and catchers, you may notice changing in their mechanics.
With baseball players, especially pitchers and catchers, you may notice changing in their mechanics.
Catchers will tend to shift weight to one side (typically away from the side in which they experience pain) while in a crouch, or they will stand up more often between pitches to release pressure on the joint.
In pitchers, you will notice a decrease in leg lift with their wind up. When huddling around the coach for a meeting, these athletes will probably be standing as opposed to kneeling.
In the weight room, it will not be uncommon for these athletes to change from a squat clean to a power clean. Catching the weight in a
deep squat position will feel extremely uncomfortable, leading the player to want to catch it in a higher, less painful position (i.e. the
power clean and power snatch position).
Even with squats, these athletes will seem to not descend as low. It is not out of being lazy at all, and when asked they will probably say “I can’t go that low.”
Is Hip Impingement Caused By Low Flexibility?
No, not at all. It is an issue of trunk/ pelvis stabilization. The athlete cannot hold the pelvis in the proper position through motion and while loading.
It’s important to realize, as a coach, that each athlete’s strength and conditioning program should be individualized.
Athletes with deep front side groin pain will not be able squat as deep, but this does not mean we need to force them into this extreme range of motion. Over time, this will actually damage the hip and land the player in a sports medicine clinic.

Why Does Squatting Deep Hurt My Hip With Hip Impingement?
As the athlete descends into the squat, notice the motion occurring at the hip. Flexion is the main one, but even with the slightest knee cave we can see adduction and internal rotation. That positioning of the body is essentially a standing version of one of our positive orthopedics tests called Scour’s Test.
Things you can look for are:
- trunk position – are they forward or leaning?
- anterior pelvic tilt – in contrast the butt will seem to stick out more
- knee cave – “knock knee”
- adduction – are the knees stacked over the feet still?
- foot contact with the ground – if they look uneven or asymmetrical something is going on above them too.
Take note of the athlete’s feet. If they are pointing straight forward perhaps you suggest a little bit of a wider stance with some external foot flair. It is important to realize with hip impingement the structures being damaged are cartilaginous in nature. Cartilages have very low vascularity and healing potential.
Let’s not crush these structures!
Modifications in squat stand will help dramatically, as will some well-spent, one-on-one coaching time to clean up the squat overall.
There’s no reason to have these athletes continually traumatize structures for the sake of getting extra range of motion in a deep squat. Remember femoroacetabular impingement can create and become labral tears of the hip, which then are probably surgical cases.
Types of Hip Impingement
Femoroacetabular impingement can be broken down into 3 types.
- Cam type
- Pincer type
- Combined
With Cam Impingement the femoral head is not as round as it should be. Remember the femoral head is the “ball” of the ball-and-socket hip joint, and ideally it should be round.
In this type of impingement, the head cannot rotate smoothly within the socket since it is not round. It is called a cam deformity because of the boney bump that forms on the outer rim of the head.
This extra bone will grind against the cartilage.
The development of a cam lesion can be associated with having a very active younger athletic career, before the closure of the growth plates in the femur.
Cam type impingement is more common. It is even said the femur takes a pistol grip appearance, otherwise known as a pistol grip deformity.
So, a question that all of the parents with pre-pubescent children who participate in year-round, single sports might ask themselves is this:
“Are we putting our children at risk of hip pain from this?”
Studies have strongly suggested we could be. Cam deformities are more common in males. As a side note, it has been found that cam deformity is considered normal to a certain degree within non-systematic populations of young healthy adults.
With this type of deformity, it is hard for the femoral head to move normally within the socket/ acetabulum. These abnormal mechanics of the hip lead to pinching and fraying of the fibrocartilage/ labrum. Fraying of the labrum can decrease the amount of proper centering of the ball within the socket, creating lesions or degeneration to the articular cartilage on the head of the femur.
If we consider where the bone abnormality develops, then Pincer impingement is almost the opposite of cam.
In a Pincer Impingement, the extra bone extends over the normal rim of the socket, or acetabulum. The labrum or fibrocartilage can be crushed underneath this extra bone prominence, and can lead to fraying of that structure, as well as groin pain.
Pincer impingement is more commonly found in females, and more associated to hip dysplasia. Hip dysplasia is a developmental condition where the socket is not as deep as normal. Pincer type impingement has also been correlated to complications after osteotomy surgery, which is meant to correct hip dysplasia, as well as abnormal positioning of the hip called retroversion.
A combined hip impingement is just that. It has aspects of bone and growth on the femoral head/ ball, as well as bony growth on the socket/ acetabulum.
Diagnosis of Hip Impingement
Proper diagnosis of femoroacetabular impingement usually includes orthopedic testing and diagnostic imaging.
The orthopedic testing typically involves:
- Impingement Sign
- Posterior Inferior Impingement Test
- Scours’ Test
- FABER’s test (flexion, adduction, and external rotation)
All orthopedic tests have different ranges of sensitivity and specificity, usually leading to a primary diagnosis of femoroacetabular impingement. However, it cannot be confirmed unless we have supporting images.
Other Possible Diagnoses with pain patterns similar to femoroacetabular impingement are:
- Hip Labral Tear
- Snapping Hip Syndrome
- Iliopsoas tendonopathy
- Iliopsoas bursitis
- Arthritic conditions of the hip joint
- Joint Infection
Diagnostic Imaging of Hip Impingement
Diagnostic imaging is typically requested in this order when going through the insurance game:
- Plain Film radiographs (aka x-ray)
- MRI – will not always show aspects of impingement
- MRI Arthrogram – typically tell you with very high certainty, if impingement or a labral tear is present
- Musculoskeletal Ultrasound (aka Dynamic Ultrasound Imaging, MSKUS, MSUS) can see aspects of impingement.
- POD CT scans – position of discomfort computed tomography

The best methods of imaging are usually performed last because they are more expensive than plain film radiographs. However, Ultrasound is now becoming a more commonly requested first test, especially when the healthcare provider is not concerned about any bony changes (i.e. arthritis, cancer, infection, etc).
Most athletes, who are at risk of hip impingement, do not often show any signs of bony changes, leading to its growing popularity. Most cases are investigated when the athlete is under 30 years old.
When using plain film radiography to diagnose femoroacetabular impingement, usually we use the A-P or anterior to posterior review first. The coccyx bone should point directly over the pubis symphysis showing us that there is a lack of rotation in either direction. Anterior to Posterior views can also assess for the presence of cam deformities (flattening of the head neck junction of the femur), degenerative changes, and cross-over sign, all of which can be indications of pelvis position.
Cross-over sign has been found in studies to be a reliable and easy way to see acetabular rim placement in an A-P x-ray10. This is helpful because you can see the relative position of the socket and then determine whether it is optimal or not.
In the past, measurements of the alpha angle were a very hot topic in regards to its accuracy in predicting femoroacetabular impingement. Alpha angles were used to quantify cam deformities on plain film radiographs and MRI. However, there have been some questions in regards to the inter-examiner reliability of the measurements.11
Are these angles consistent amongst multiple techs reading the same image?
Can these measures be duplicated over and over again?
One study, published in 2008, found a very low correlation between pain and radiographic findings of femoroacetabular impingement.13 The study found a much higher prevalence of larger alpha angles in men. In women, this study found that cam deformities were more common than pincer deformities. Historically, women have suffered more from pincer variety of impingement.
If there’s suspicion of femoroacetabular impingement after receiving plain film radiography (x-rays), the patient should be referred for an MRI or MRI Arthrogram.
MRI Arthrogram is a more direct approach to finding and/or confirming femoroacetabular impingement or labral tears. However, it’s not uncommon for patients or athletes to have the MRI done first.
What is the difference between MRI and MRI Arthrogram imaging?
MRI Arthrogram procedures require contrast dye to be injected into the joint space, revealing more detail of the joint, the labrum, and the underlying cartilage.
The contrast dye will usually show thinning of the articular cartilage, however it will seldom penetrate deep enough to show delaminating articular cartilage. In conditions where labral tears are expected, this contrast dye highlights any frays or tears within the fibrocartilage.
Diagnostic Musculoskeletal Ultrasound is a good tool to use within health care offices for various good reasons:
- low barrier of entry
- low cost
- dynamic/movement imaging
- shows the labrum
- shows the muscles, tendons, ligaments, and joint capsule
- no exposure to radiation (safe for adolescences and pregnant females)
In many cases, the cost of an MRI is more than double that of an Ultrasound. Both yield around the same specificity and amount of information on the joint being imaged. The current gold standard is the MRI Arthrogram, however the MRI Arthrogram typically costs more than 4 to 5 times the typical cost of a Diagnostic Ultrasound.
A study in 2009 showed Ultrasound could even be a viable option in diagnosing labral tears of the hips. Ultrasounds produced a sensitivity of 94%, which is only 6% behind the 100% of the MRA.8
Diagnostic ultrasound will effectively reveal any possible pathology within the muscles, tendons, ligaments, and extracapsular area around the joint space. However, it is limited and cannot investigate deep inside the joint space where an MRI Arthrogram would.
However, many sonographers educated in musculoskeletal ultrasound, can image anterior capsular effusion, as well as discontinuity, or heterogeneous appearance of the anterior labrum. Granted, this does not rule 100% in-favor of a labral tear or femoroacetabular impingement, but it does give us great information to use for program design that will optimize recovery in the rehab setting.
Diagnostic Musculoskeletal Ultrasound is a dynamic image. An experienced sonographer can place the probe on the anterior side of the hip, where the pinching is located, and flex the patient’s hip into flexion/rotation to see if the pinching occurs. The beauty of this is that we get to see the joint under motion, whereas in an x-ray, MRI, and a MRI Arthrogram we cannot.
The dynamic aspect of Musculoskeletal Ultrasound is one of the unparalleled benefits to using this method of imaging over other types. It is safe, effective, cheap, and provides much information that can help the treating physician do their job more effectively. It’s important to note that there is no amount of radiation involved in diagnostic ultrasound imaging, so it is safe for pregnant females as well as adolescents.
Position of discomfort CT scans can be used to assess a 3D image of the surface of a bone that might require surgical reconstruction. When putting the patient into a position of discomfort (often supine flexion, internal rotation and adduction), the scan can reveal a positive finding of narrowing of the joint space. Putting the patient into a position of discomfort (often supine flexion, internal rotation, and/or adduction), allows for the scan to positively reveal any presence of joint space narrowing. This narrowing would indicate a mechanical impingement. 14
Some sources say position of discomfort CT is the best way to demonstrate bony impingement lesions, but it is not the best way to visualize labral pathology or other soft tissue problems of the hip. In these cases, we would look to a MRI, MRI Arthrogram, or Musculoskeletal Ultrasound.
Treatments for Femoroacetabular Impingement
Treatments for femoroacetabular impingement will vary based upon the severity of your symptoms.
Treatments can include:
- avoidance of motion or rest
- increasing range of motion
- increasing strength
- improving core strength/control
- improving gait
- injections within the joint space
- non-steroidal anti-inflammatory medications
- surgery

Femoroacetabular Impingement is more prevalent within the young population, and, many times, avoidance of activity is not a realistic option for these athletes. For this reason often times surgery can be helpful.
Now let’s recap on each section of traditional treatments. Avoidance of activity/motion is very important in decreasing the amount of symptoms and/or localized inflammation at the anterior aspect of the hip joint. Generally speaking, if you feel pain, then you will not move well in rehabilitation.
The initial part of therapy is focused on increasing pain-free range of motion. The next goal is to increase local strength/stabilization, trunk stabilization, and apply what the patient gains in an open chain (feet off the ground) position to a closed chain activity (feet on the ground). If all of this fails, then surgical intervention can be an option.
How Does Hip Impingement Affect Pitching?
Pitching with femoroacetabular impingement will lead to lack of front leg mechanics, as well as inconsistencies in velocity and ball placement. Rotator cuff tears and labral tears can also follow.
Often, since femoroacetabular impingement is found in asymptomatic, or non-painful, populations, it is not unreasonable to think that we can also decrease pain in cases of minor impingement in baseball players and/or young athletes. However, when cases are non-responsive, or when pain persists around the groin, it is always important to confirm that there is no labral or fibrocartilage tearing within the hip.
Improving non-painful range of motion in the hip is often accomplished with a manual therapist, physical therapist, physiotherapist, or sports chiropractor. This is where the practitioner assists the athlete in increasing their non-painful range in motion through a variety of exercises or manual therapies.
Examples of some techniques used by clinicians in this setting are:
- Myofascial release (hands or instruments)
- Neuromuscular re-education
- Active-assisted range of motion
- Biofeedback of motions
Generically speaking we call these “re-educating movement patterns.” When strength training an athlete with femoroacetabular impingement, the overseeing practitioner should consider the activation of muscles around the hip and pelvis. Some of those muscles include the gluteus maximus, gluteus minimus, iliopsoas, muscles of the core/trunk, and external rotators of the hip, to name a few.
Some research suggests that strengthening the mid-range of hip flexion and extension should be done first since this is the range where the athlete does not experience pain. It is also important to achieve optimal gluteal activation to help reduce the muscular activity of the iliopsoas/hip flexor and tensor fascia latae (TFL).
The iliopsoas and TFL are often activated during the compensatory patterns that surround femoroacetabular impingement. It is important to keep in mind, however, that when following this methodology, the iliopsoas and hip flexor region still need to be strengthened. Increasing the strength of these muscle groups helps to reduce anterior hip joint forces during active hip flexion. If the iliopsoas is not adequately strengthened, often times the TFL will become dominant in hip flexion.
This TFL dominance increases the amount of internal femoral rotation.
During the initial stages of rehabilitation, limiting activities that involve hip flexion is advised due to the muscle’s local proximity to the joint space. Irritation of the tendon or the hip flexor can result in secondary inflammatory effects around the joint space.
When the goal of rehab is to gain control over gait abnormalities, it is often important to give the athlete feedback on any shifts in where he or she bears the weight, especially in the frontal plain.However, all planes of motion are important when re-training gait and strengthening the hip/pelvis.
The frontal, sagittal, and transverse planes are all extremely important. Therapists will often choose to train this in an open-chain position with added perturbations.
From a theoretical perspective, if the athlete can control the hip, pelvis, and torso in an open-chain position, then we can begin to move them to a scaled approach of weight-bearing exercise. Ground exercises in rehab are the least weight-bearing, while a full standing position lies at the other end of the weight-bearing spectrum.
Typically, athletes with less severe femoroacetabular impingement can start with more advanced weight-bearing positions, while others who have had surgery will typically need to start with the basics.
When improving range of motion in an athlete, passive range of motion is the usual starting point, especially before active range of motion.
Passive range of motion encompasses motions where we do not require the athlete to use their own muscles to accomplish that range of motion.
Active range of motion occurs when they do use their muscles to move the joint.
Typically patients with femoroacetabular impingement have a loss of passive motion, which will translate into a loss of active motion.
A good starting point to improve the range of motion is to start by working on the passive motion first. This can be done in a variety of ways.
Here are a few options to improve passive hip motion:
- Band-assisted
- Active-assisted range motion
- Deep tissue manual therapy
- Static stretching
- Injection therapies
- Non-steroidal anti-inflammatory medications
It is difficult to normalize joint mechanics and muscle activation patterns until pain increases with normal range of motion.
It is not uncommon for athletes to resist using injection therapies or non-steroidal anti-inflammatories. However, to properly rehabilitate the hip/torso region, we need to accomplish pain-free passive motion first.
Femoroacetabular Impingement Surgery Options
Open Hip Dislocation Surgery
When all else fails, some cases will require surgical intervention for femoroacetabular impingement Types of procedures your athlete may be presented with are open hip dislocation, reverse periarticular osteotomy, the direct anterior “mini open approach”, and arthroscopy surgery for femoroacetabular impingement.
The open hip dislocation procedure was one of the first methods of surgical treatment and satisfactory results have been reported in clinical settings for surgical hip impingement patients who are 5-10 years post-op.
Surgical hip dislocation is often a preferred technique when the patient has had either Legg-Calvé-Perthes disease or Slipped Femoral Capital Epiphysis (SFCE), both of which are childhood and adolescent conditions.
The main reason why the athlete would be at an advantage with this procedure is that there is a possibility that a trochanteric advancement can be performed, as well as a relative neck lengthening. Both of these can optimize the functioning of the adductors.
Some counter-indications for using surgical hip dislocation to correct femoroacetabular impingement are:
- Smokers
- Anterior- Posterior cartilage damage
- Extensive cartilage damage
- Anterior Hip Dislocation
- Patients over 40 years of age
Reverse Periarticular Osteotomy Hip Surgery
The Reverse Periarticular Osteotomy (Reverse PAO) is usually used for cases of pincer femoroacetabular impingement, where a true acetabular retroversion is secondary to an external rotation deformity. Some criteria for inclusion for this procedure are found on radiographic evidence:
- Cross Over Sign
- Posterior Wall sign
- Ischial Spine Sign
Arthroscopic surgical intervention for femoroacetabular impingement has risen 600% since 2006.
One recent systematic review even cited this as the “preferred technique.”20
In 2006 the arthroscopic technique was used for the first time to correct osseous (bone) deformities found in femoroacetabular impingement. The major difference between this type of procedure and a surgical hip dislocation is there is no need to dislocate or remove the ball from the socket of the hip.
Direct Anterior “Mini Open Approach” Hip Surgery
The direct anterior approach for open treatment of anterior femoroacetabular impingement claims to be an improvement over the open surgical hip dislocation. The idea is to improve recovery time by not disrupting the trochanter or the adductor mechanism. Recovery times from different types of hip procedures for femoroacetabular impingement can vary. 21
With less invasive hip arthroscopy, athletes in good health can return to play within three months. However, the worse your health is prior to going into surgery, the longer the recovery time can be. To put it simply, the better muscular strength/conditioning the patient has prior to the procedure, the less time it will take them to recover.
Post-Surgery Rehabilitation Of The Hip
Post-Op Rehabilitation typically follows 4 phases
Phase 1 encompasses the first 3-weeks post-op and the goals of this period are to increase passive range of motion, and to protect the joint from acute inflammation and re-aggravation.22
Phase 2 typically revolves around restoring full range of motion of the hip and improving non-compensatory gait. In other words, working on increasing the hip motion and improving normal walking mechanics. 22
Phase 3 tends to be more fun for patients. This phase works toward increasing strength in the trunk and lower extremity, and ideally restoring both of those areas back to pre-operative status, or better.22
Phase 4 is where the athlete starts to incorporate more complex drills such as plyometrics, agility training, and more sports-specific activity. 22
Each phase generally last about 4 weeks, however they can take longer based upon your athlete’s progress. During phase 4 it’s important to have open communication between your physical therapist/ physiotherapist/ sports chiropractor and the skills coach, as well as your strength and conditioning coach. Athletes who play at high school and college levels, can tend to fall behind on skills and plyometrics if there is a lack of communication between the health care professional(s), the strength coach, and the coach.
As a strength and conditioning coach, it is important to stress the need to strengthen the body around the injury. Naturally, the hip joint will need time to heal itself after the trauma it has been through, however, the rest of the body is full capable of some level of sports-specific activities. This can even result in the athlete returning to play faster.
If we are considering a baseball pitcher, this athlete should be participating in shoulder-prevention exercises or rotator cuff exercises to keep the areas of the upper extremity conditioned while the lower extremity is healing from the surgical procedure.
Article References
1. Clohisy JC, Baca G, Beaulé PE, Kim Y-J, Larson CM, Millis MB, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med (2013) 41(6):1348–56. doi:10.1177/0363546513488861
2. Takeyama A, Naito M, Shiramizu K, Kiyama T. Prevalence of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int Orthop (2009) 33(5):1229–32. doi:10.1007/s00264-009-0742-0
3. Nepple JJ, Vigdorchik JM, Clohisy JC. What is the association between sports participation and the development of proximal femoral cam deformity? A systematic review and meta-analysis. Am J Sports Med (2015) 43(11):2833–40. doi:10.1177/0363546514563909
4. “Josh Beckett’s Hip Impingement Injury.” Beyond the Box Score. N.p., 10 July 2014. Web. 21 July 2016.
5. “Devin Mesoraco’s Tragic Hip.” Redleg Nation. N.p., 23 Apr. 2015. Web. 21 July 2016.
6. Gaines, Cork. “Alex Rodriguez Is on Fire at Age 39, and a ‘miracle Surgery’ He Had in 2013 Is a Huge Reason Why.” Business Insider. Business Insider, Inc, 20 Apr. 2015. Web. 21 July 2016.
7. Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248.
8. Troelsen, Anders, Inger Mechlenburg, John Gelineck, Lars Bolvig, Steffen Jacobsen, and Kjeld Søballe. “What Is the Role of Clinical Tests and Ultrasound in Acetabular Labral Tear Diagnostics?” Acta Orthopaedica 80.3 (2009): 314-18. Web.
9. Banerjee, Purnajyoti, and Christopher R. Mclean. “Femoroacetabular Impingement: A Review of Diagnosis and Management.” Current Reviews in Musculoskeletal Medicine Curr Rev Musculoskelet Med 4.1 (2011): 23-32. Web.
10. Jamali, Amir A. “Anteroposterior Pelvic Radiographs to Assess Acetabular Retroversion: High Validity of the “cross-over-sign”.” Journal of Orthopaedic Medicine. N.p., Mar. 2007. Web. 20 July 2014.
11. Nouh MR, Schweitzer ME, Rybak L, Cohen J. Femoroacetabular impingement: can the alpha angle be estimated? AJR Am J Roentgenol 2008;190(5):1260–1262
12. Panzer S, Augat P, Esch U. CT assessment of herniation pits: prevalence, characteristics, and potential association with morphological predictors of femoroacetabular impingement. Eur Radiol 2008;18(9):1869–1875.
13. Ranawat AS, Schulz B, Baumbach SF, Meftah M, Ganz R, Leunig M. Radiographic predictors of hip pain in femoroacetabular impingement. HSS Journal. Online First™, 10 January 2011 (in press).
14. Singh PJ, Pritchard M, O’Donnell J. The POD CT scan—a better way to demonstrate FAI and early hip degeneration. Annual Scientific Meeting. International Society for Hip Arthroscopy; Oct 2009.
15. Philippon MJ Decker MJ Erik G Torry M Wahoff M LaPrade RF Rehabilitation Exercise Progresion for Gluteus Medius Muscle with Consideration for Iliopsoas Tendinitis: An in Vivo Electromyography Study. Am J Sports Med. 2011;39(8):1777‐1785
16. Selkowitz DM Beneck GJ Powers CM Which Exercises Target the Gluteal Muscles While Minimizing Activation of the Tensor Fascia Lata?. Electromyographic Assessment Using Fine‐Wire Electrodes. J Orthop Sports Phys Ther. 2013;43(2):54‐64
17. Lewis CL Sahrmann SA Moran DW Anterior Hip Joint Force Increases with Hip Extension, Decreased Gluteal Force, or Decreased Iliopsoas Force. J Biomech. 2007;40(16):3725‐3731
18. Naal FD, Miozzari HH, Wyss TF, Nötzli HP.. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med (2011) 39(3):544–50.10.1177/0363546510387263
19. Weiland DE, Philippon MJ. Arthroscopic technique of femoroacetabular impingement. Oper Tech Orthop (2005) 15(3):256–60.10.1053/j.oto.2005.07.002
20. Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP.. Trends in hip arthroscopy utilization in the United States. J Arthroplasty (2013) 28(8 Suppl):140–3.10.1016/j.arth.2013.02.039 – “preferred tech – arthros”
21. Cohen SB, Huang R, Ciccotti MG, Dodson CC, Parvizi J.. Treatment of femoroacetabular impingement in athletes using a mini-direct anterior approach. Am J Sports Med (2012) 40(7):1620–7.10.1177/0363546512445883 – mini-open
22. Grzybowski JS, Malloy P, Stegemann C, Bush-Joseph C, Harris JD, Nho SJ.. Rehabilitation following hip arthroscopy – a systematic review. Front Surg (2015) 2:21.10.3389/fsurg.2015.00021
23. Lintner, D, Noonan, TJ, and Kibler, WB. Injury patterns and biomechanics of the athlete’s shoulder. Clin Sports Med 27: 527–551, 2008.
24. Fleisig, G, Nicholls, R, Elliott, B, and Escamilla, R. Kinematics used by world class tennis players to produce high-velocity serves. Sports Biomech 2: 51–64, 2003.
25. Ross, J. R., J. J. Nepple, M. J. Philippon, B. T. Kelly, C. M. Larson, and A. Bedi. “Effect of Changes in Pelvic Tilt on Range of Motion to Impingement and Radiographic Parameters of Acetabular Morphologic Characteristics.” The American Journal of Sports Medicine 42.10 (2014): 2402-409. Web.
26. Banerjee, Purnajyoti, and Christopher Mclean R. “Femoroacetabular Impingement: A Review of Diagnosis and Management.” Current Reviews in Musculoskeletal Medicine Curr Rev Musculoskelet Med 4.1 (2011): 23-32. Web.
27. Kuhns, Benjamin D., Alexander Weber E., David Levy M., and Thomas Wuerz H. “The Natural History of Femoroacetabular Impingement.” Front. Surg. Frontiers in Surgery 2 (2015): n. pag. Web.
28. “Femoroacetabular Impingement (FAI)-OrthoInfo – AAOS.” Femoroacetabular Impingement (FAI)-OrthoInfo – AAOS. N.p., n.d. Web. 09 Sept. 2016.
29. Kokmeyer D, Strzelinski M, Lehecka BJ. Gait considerations in patients with femoroacetabular impingement. Int J Sports Phys Ther 2014;9:827-838.