Is Neck Pain Impeding Your Golf Game?
Neck pain from golf can have causes that are not from disability diagnoses. Common associated diagnoses are cervical disc herniation and pinched nerve top the list. Symptoms include pain from swinging a club and looking side to side.
SYMPTOM CHECKER:
Does your neck pain get worse with:
- Stiff neck.
- Difficulty moving the neck, especially when trying to turn the head from side to side.
- Sharp pain
- Soreness in the upper shoulder
- Aches pain that travels between the shoulder blades
- Trouble lifting objects
- Headaches.
- Muscle spasms
- Reduced neck range of motion
- Reduced shoulder range of motion
- Nerve pain
- Neck Stiffness
- Muscle Aches
- Shooting or numbness traveling beyond the elbow
Neck pain can present in different severities. Based upon your seriousness and reason for neck pain, you may have only specific symptoms above.
In this article, you’ll learn everything you need to know about neck pain during golf, except for how to comprehensively treat it. We will be sharing some fantastic tools to reduce pain within a matter of days. Still, many people who attempt self-care have trouble implementing solutions.
Use the sidebar to jump around to what interests you most in this article. If you have any questions, we are here to help. Just see us in Huntington Beach, CA- it’s a great place to vacation! Pelican Hill is right down the street!
Neck pain can affect your golf game in many ways, and none of them are fun.
Pain during play can turn a game you love into a frustrating experience. It does not just ruin your fun. Neck pain during golf can mentally throw off your game and physically change it via grip strength, ability to keep your eyes on the ball, and much more.
To make matters worse, it can carry over into your everyday life and daily non-golf activities. Sleep, sitting and driving top this list. Unaddressed neck pain can also disrupt the function of surrounding joints, such as the shoulders, upper back, and even the low back and hips.
All of these things can continue to degrade the quality of your swing and often eventually create pain in other areas.
Let’s dive into what could be creating neck pain during golf.
Let’s start with the specific diagnostic conditions that could be the result of your neck pain. Then we will deconstruct what these diagnoses are and what brings them about.

Neck Pain Diagnoses
- Cervical facet joint syndrome
- Most likely cause excessive extension (looking up), compression (downward pressure), rotation (turning). We will cover what all this means in the article. Never fear.
- Cervical disc derangement
- Possible causes: posture, inefficient movement, trauma, repetitive microtrauma: compression, flexion, rotation
- Cervical radiculopathy
- Possible causes: arthritis/intervertebral foramen (IVF) stenosis, disc herniation from factors that cause disc derangement: excessive compression, flexion, rotation
- Hypermobility syndrome
- Possible causes: congenital (genetic)/trauma/repetitive microtrauma
- Ligament laxity
- Causes: posture, repetitive microtrauma, trauma
- Dynamic instability
- Cause: considerable trauma
You might be wondering about postural issues or “imbalances,” which are not included in the list, only because they are technically not a medical diagnosis. Still, they can certainly be a contributing factor to what caused the diagnosis and tissue disruption.
Also, “myofascial pain (muscle pain)” is usually a finding, not a diagnosis that is most often another symptomatic byproduct from one of the above diagnoses. These are more contributing causes to the diagnosis or neurological compensations as a result of the diagnostic condition, but not the diagnosis itself.
As complicated as it may sound, you can get better very quickly. Check out this golfer’s testimonial of chest pain (from his neck) that was stopping hip from golfing. Another happy customer!

Cervical Facet Joint Syndrome
Do chiropractic adjustments feel good, but don’t last?
That sounds like the typical story with facet based pain in the neck. Many golfers describe their neck as “feeling stuck and needing a neck adjustment,” which only helps with part of the puzzle.
It’s beneficial to improve the endurance strength of the deep neck flexor muscles of the neck to ensure you don’t have to keep going back for a weekly adjustment. I’ll cover this a bit more in detail later, so stay with me.
The disc between two adjacent vertebrae is not the only joint that connects one vertebra to the other.
On the backside of the spine, there are two joints on either side of the vertebra where the two adjacent vertebrae join directly to one another. These are the facet joints.
With movements involving extension (looking up) and rotation, these joints can become overly compressed and inflamed. This problem can be solved very quickly if you find the right person.
Note: If the doctor you’ve seen so far took less than 5 minutes before suggesting a solution, please find a better doctor for your sake. Choosing the right doctor as your guide overcoming neck pain comes down to if they take the time to know what your body needs. If they don’t sit down, ask you questions, and manually test your neck, they will recommend poorly, leading to unfruitful treatment.
Adjustments can help with the reduction of pain. Still, to really “hit the save button” on your progress, you’ll need to do some focal therapy exercise for the deep neck flexors, mid-back, and shoulder blade region.
Soft tissue manipulation can also be a part of the puzzle, depending upon length of time with neck pain, when you feel it in your swing, and what time of day it’s worse/ better.
A thorough exam and history (which may take over an hour) by a sports chiropractor, physical therapist, or medical doctor, will help guide you to what works best for you.
Under the right guidance, many of these conditions of the neck can improve significantly within 5-6 patient visits (and many times shorter to be honest). Creating an exact, long-term, at-home plan will take a few sessions.
As we tell all of our patients, if you are not confident you’re getting better, then you have not found the correct solution to your neck pain. That confidence in knowing can come within just a few weeks.
Let’s jump into another common reason for neck pain after golfing.
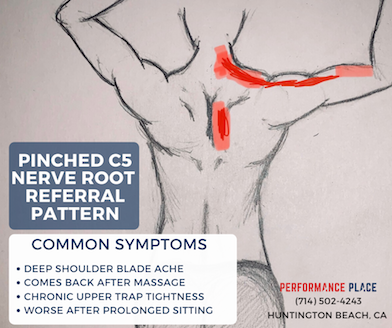
Cervical Radiculopathy
This condition happens when the damaged disc displaces backward or herniates posteriorly; when this occurs, it can compress the nerve roots exiting the back of the spine.
It will cause pain in areas away from the damaged tissues. Anywhere that the nerve goes through the neck, or into the shoulders, or upper back, and even arms can present with:
- Pain
- Tingling
- Achiness
- Prolonged soreness
- Stabbing
- Shooting
The pain or discomfort often presents in locations far from the injured tissues. Each nerve root has a different pathway of pain presentation.
This injury occurs from insults of flexion, rotation, and compression. Rotation is frequent in golf as your body turns under your head (looking at the ball). For that reason, this occurs in golf more common than you’d think, yet it is easily treatable if you catch it within the first month.
Hypermobility Syndromes & Ligament Laxity
Hypermobility occurs through trauma (whiplash), repetitive microtrauma, be congenital (genetically born with), or some combination. There’s a broad spectrum of hypermobility disorders that run the gamut from minor to severe to debilitating.
These conditions lead to ligament laxity and reduced elasticity of the ligaments, making the cervical vertebral unstable, which can cause all kinds of dysfunction and pain presentations. For this reason, you may be presenting as a cervical disc injury (see above symptoms), but caused by spinal instability.
These situations are a little more complicated than other types of neck pain diagnosis, but a reduction of pain is certainly a probability.
Dynamic Instability
Dynamic instability is a medical condition where one joint becomes significantly hypermobile and very unstable. The instability is due to a past significant trauma that tore or significantly damaged the ligaments of that particular joint.
It is more local/ isolated and less global than hypermobility syndromes.
It is a partial dislocation of one vertebra over another.
Dynamic instability can be severe enough where there can be brainstem or spinal cord compression on top of nerve root compression and disc damage. When spinal cord compression becomes involved, this becomes a much more severe condition.
Causes
What causes these issues to occur?
With all of the above-listed diagnoses, there are reasons why they start in the first place. Normal structures under normal situations don’t tend to hurt. Most of this can be found through detailed history taking process that tends to unveil why you are in pain in the first place.
Here is a shortlist of possible reasons for neck pain.
- Postural issues which contributed to cumulative, repetitive microtrauma carried over from inefficient movement
- One-sided repeated rotation movement that causes imbalances which contributed to cumulative microtrauma
- One-sided, repeated rotation movement with poor posture
- Congenital connective tissue disorders
- Trauma, like past car accidents
- Usually some combination of the above
Treatments Options
Successful treatment depends on your unique reason for neck pain. As you can see by the prior lists, there are many reasons for neck pain. The most common are disc irritation, radiculopathy and cervical facet joint syndrome.
Successful treatment should yield a near complete reduction of pain through day-to-day activities within under 2 weeks. Treatment may be longer to build tolerances to quick movements, like swinging a golf club.
Rehabilitation of the neck and shoulder girdle takes time. The muscles and joints must be challenged to stimulate positive adaptations. The body will build a buffer against re-injury when corrective rehabilitation exercises are done 3 days a week.
There are many pain reducing treatments out there, but many of these provide short-term relief. There are situations where these treatments work extremely well, yet they tend to become overutilized as a last ditch option. None of them force the body to build buffers against re-injury, which is why people sometimes experience short-term success with these methods.
- Adjustments
- Massage
- Soft tissue mobilization
- Traction
- Numbing lotions
- Ice
- Heat
- Rest
The following video demonstrates a self treatment method that has proven to work extremely well in over 50% of people I’ve used it with. I was very surprised when it kept working for my patients. At the time I was a soft tissue doctor and did all of the things I listed above as primary treatments. Long story short, they weren’t working so I decided to offer something new.
When this exercise works, it simply means the muscles are not the primary issue. A cervical disc or nerve pressure is. Following this exercise, we ALWAYS suggest building the neck and shoulder blade buffers to keep going the right direction in the first few weeks of care. No corrective exercise should be painful. You’ll know you have the wrong rehabilitation pain when it hurts to perform the exercises.
When this exercise works, it means we have a rehab case on our hands and should only become surgical if 6+ weeks of clinician supervised care is not successful (which is rare).
The Complicated Topics
FUNCTIONAL ANATOMY AND BIOMECHANICS OF THE NECK
In this section, we will be getting into the nitty-gritty of anatomy and biomechanics. This section is intended to better inform those who seek this type of information, but if this is not you don’t worry. You don’t need to know every little thing about how the body works to feel better. We do though. If you are struggling to find relief from your neck pain just reach out to us. There is a “Book Now/ Calendar” on the site that can help you be seen by a doctor who will give the direction you need.
Even if you feel you’ve tried everything, we have had amazing results helping people get fast relief.
Now onto the tough stuff…
First, let’s explain the unique biomechanics of the neck so you can better understand what will make you better without falling into the trap of months of unsuccessful treatment.
Just like the spine, the neck has two curves. In your back, you have an extended/arched curve of the lumbar (lower back) spine (lordotic curve), and a more rounded/flexed curve of the thoracic (upper back) spine (kyphotic curve).
The neck has double curvatures that should mirror the curvature pattern of the back. Where the mid and lower neck vertebra, 3-7, more extended, like the low back and upper neck vertebra, 1 and 2, more flexed, like the middle and upper back.
The picture on the right below demonstrates this.
However, due to poor posture, this curve often reverses over time, as demonstrated in the picture below (left).
So, let’s review our mechanisms of injury.
We had extension and rotation that irritates the facets and closes the IVFs (the holes that the nerve roots pass through to exit the spine). We also have flexion and rotation that damages discs and nerve roots.
Now let us consider a fascinating characteristic about the first two vertebrae of the neck that differentiates them from all other vertebrae in the body. The first two neck vertebrae have no disc between them, and as such, flexion with rotation cannot cause any disc damage at these joints.
Further, when C1-C2 is in flexion, it puts C3-C7 into mild extension, protecting the discs in the rest of the neck.
Now let’s talk about the muscles of the neck and their function.
Muscles that flex the neck are on the front side, whereas muscles on the back extend the neck.
There are layers of these muscles on the front and back of the neck from deeper to more superficial.
The deeper muscles are much smaller, and the more superficial/ surface deep muscles are much larger. The deep neck flexors, on the front of the neck, retract the chin and head backward, putting the upper two vertebrae into flexion (refer to the picture on the right above).
The more extensive superficial (more surface deep) neck muscles pull the chin and neck down towards the chest, putting all the vertebra in the into flexion, let’s not worry about those for now.
It is the deep neck flexors that become inhibited with poor posture, allowing the chin to jut forward. This posture causes the mid and lower vertebra to set in a chronically flexed position, compressing the front of discs, which pushes them backward.
Don’t worry; it is possible to “re-activate” these inhibited muscles via specific exercises biasing these muscles within motion. We will get to that later.
Now take that flexed neck position and rotate it (look back and forth) quickly over and over again. We could be heading down a path we don’t want to travel with aches and pain at the end of that road.
Another cool thing about the deep neck flexors is that they also affect the positioning of the upper back.
If we recall, the upper back has a natural structural rounding to its architecture. And because of our modern lifestyles, this rounding tends to increase over time, further contributing to poor posture and undesirable disc stresses.
Further, while the upper back further rounds, the chin juts out, also leading to further inhibition of the deep neck flexors. Again this is treatable, so don’t worry we will get to that!
There are many reasons for this, including neurological reflexes such as the ‘righting reflex’ and ‘pelvo-ocular reflex,’ and even foot and ankle positioning, fascial tensioning of muscle spindles, etc. The body is amazing when it comes to some of these natural reflexes. Consider your morning coffee helping with your morning DM!
But for the sake of simplicity, let’s stick with the basic biomechanics of the neck. Just know these reflexes are normal, yet can sometimes trigger types of pain in the process.
Okay, now to get a little techy! If we recall, when we retract the chin (making a double chin) with the deep neck flexors, the mid and lower neck vertebrae extend. The muscles that extend the middle and lower neck vertebra travel down past the neck and insert into the mid and upper back, as low as the 6th thoracic vertebra.
As such, these muscles tension to respond to retraction of the chin, there is an extension torque that travels directly through the 4th thoracic vertebra. This torque pulla the chest up and reduces upper back kyphosis/rounding, putting us in a more mechanically advantageous position as well as further reducing stress on the neck.
Packing the chin also will prevent full neck extension and compression through the cervical spine during the rotation and maintaining a straighter and more extended upper back throughout the swing.
Then by adding chin retraction with shoulder blade depression, the lower cervical vertebrae will also gap, creating space between the joints and reducing the risk of facet irritation.
Look at Rory Mcllroy at the end of his swing.
He isn’t looking up through his neck in the rotated position. His neck is stacked and packed while he is looking up because of his thoracic/mid-upper back extension, not from upper neck extension.
This type of mechanics through a golf swing allows us to play without neck pain, arm numbness, or an ache between the shoulder blades.
Now, this may all seem pretty complicated. Still, it is actually an oversimplification of all the variables and factors involved in the dynamic mechanics engaged in restoration and injury-causing mechanisms.
The human body, and how it executes tasks, is relatively complicated.
While postural adjustments can sometimes help prevent injuries to the neck, they often aren’t enough to fix tissues once they’ve become damaged or inflamed. There are specific treatments to be discussed.
Such as nerve gliding treatments for radiculopathy.
Centralizing and stabilizing treatments for disc derangements.
Specific reeducation movement therapies
Soft tissue work to iron out imbalances, compensations, and adhesions that have developed as a response to the injury or irritation.
Joint mobilizations for joint capsule adhesions.
Reeducation of the nervous system.
It can be a complex and dynamic process, where initial movement treatments that rid symptoms can create compensations that need to be changed as well.
Everyone is different and requires unique individual fine-tuning.