Case Study: Piriformis Syndrome
Reduced By 50% Within 3 Days. Running Again Within 2 Months
By Dr. Sebastian Gonzales, DC, DACBSP®, CSCS
The conversation. The healthy motivation. The delicious breakfast that followed Saturday morning workouts. Jill loved everything about her running and cycling groups. An ironman triathlete in her mid-50s, Jill had been running for two decades.
When her running friends started getting into triathlons, they signed up for new races together. Their first full Ironman Triathlon was Tempe. Since then, they’ve done at least one per year!
For Jill, swimming, biking and running routines weren’t just exercise. They were her social time; a chance for her to catch up with friends. So when her piriformis syndrome became so painful that she could no longer run, she knew she needed to take action.
Jill came to Performance Place® Sports Care after nearly a year of unsuccessful attempts at reducing her piriformis syndrome pain. Having treated minor injuries for Jill before, I knew proper guidance—and her recovery mindset—would get her back in action.
How It All Started
About a year ago, Jill began to develop right-sided buttock pain. There was no trauma involved: no falls, nothing she recalled doing that would have created the pain.
Unsure where the discomfort was coming from, she turned to the Internet for answers.
After countless hours of research, Jill self-diagnosed her buttocks pain as Piriformis Syndrome. Like most runners with this condition, she continued her exercise routine, convincing herself the pain would go away on its own.
For the first two months, her hip was only achy when she was running or biking. She didn’t experience any pain when sleeping, doing dishes, putting on shoes or sitting. It didn’t affect her day-to-day activities, as the condition often does in more severe cases.
But the pain didn’t go away. Instead, the deep ache in her piriformis began to creep into her daily life.
Jill would feel great when she opened her eyes in the morning. But as soon as she got out of bed, her piriformis muscle would begin to ache intensely. Over time, this single step out of bed became a source of excruciating pain, often taking her to her knees. The pain would last for about 30 minutes as she completed her morning routine of washing dishes, feeding her dog and walking to her car.
Within the first five minutes of her half-hour commute, Jill’s discomfort would begin again. Sitting in traffic was so uncomfortable that she felt the need to wiggle around in her seat as if to get pressure off her right hip. And when she finally got to work, she wasn’t able to walk from her car to her office without feeling pain in her right hip.
After the initial pain subsided, Jill would feel good for most of the workday—as long as she wasn’t bending over or sitting for too long. But by the time she reached home every evening, her commute had exacerbated the ache once more.
Each morning, she would wake up and begin the cycle all over again, starting with that first painful step out of bed. On weekends, she would show up late to her running events so that she could still see her friends at their post-workout breakfast.
Jill could barely walk, let alone run. She lived like this for 11 months.
What Didn’t Work
You may be asking yourself, “Why didn’t Jill go to the doctor if it got so bad?”
She did. In all, Jill tried three chiropractors, two massage therapists, a trio of orthopedic surgeons and even an acupuncturist.
She underwent between 50 and 60 chiropractic care sessions, which consisted of chiropractic adjustments, chiropractic massage, active release, Graston, spinal decompression and exercise therapy—each delivering results that failed to last beyond an hour. Massage therapy had worked wonders for her running friends, who had used the treatments to deal with plantar fasciitis and hip pain. But although massage seemed to give Jill more release than her chiropractic treatments, her piriformis pain returned every morning. She had experienced no real improvement after 10 massage therapy sessions.
Then, quickly running out of options, Jill began wondering, “Maybe I need surgery to fix piriformis syndrome.” It’s what many of us would think if we were in her position. But even after her friends, family and chiropractors firmly advised her to consider surgery, the idea didn’t sit well with her. With MRI results in hand, Jill approached three different orthopedic surgeons, hoping they would provide a clear answer. But each surgeon offered a different opinion.
Frustrated, confused and still unable to do what she loved, Jill felt hopeless. After 11 months of limited success, she considered giving up running forever—until she decided to try something different.
Helped Relieve Piriformis Syndrome Pain
Visit #1 At Performance Place® Sports Care
With new patients, I’ll typically ask about their goals and passions to ensure I suggest the most suitable treatment for their needs. Although I had seen Jill for a few minor running-related injuries in the past, I asked her several questions to make sure her mindset hadn’t shifted.
- Do you run because you love it, or are you doing it to accomplish another goal such as weight loss or mental calmness?
- If your pain went away tomorrow, what’s the first thing you would do?
- If 100% of your pain went away, would you have any fear of it returning?
- Do you believe your piriformis pain to be a permanent problem or a temporary bump in the road?
- Do you consider yourself broken in any way, shape or form?
Jill’s answers were the same as when I first worked with her. She runs because she loves the way it makes her feel, spending time with her friends and experiencing nature. The first thing she wanted to do once she was pain-free? Run a few miles with her friends. Then, sit with them at the post-workout breakfast table without her piriformis feeling like an icepick the entire time.
She did have concerns that her piriformis pain could return, but it was because so many doctors had told her that her running days were over. She ultimately believed she could overcome it. She was not broken; this was a minor bump in the road.
Jill’s recovery mindset was an invaluable asset for our work together. It helped me guide her to her solution faster than if she had thought part of her body was permanently damaged and beyond repair.
Her examination during Visit #1 lasted about 1.5 hours. We talked, tested and re-tested to confirm we were starting off in the right direction. At this point in her condition, there was no need for spinal adjustments, massage, tissue work or stretches. She had tried all of that already, with minimal results. Instead, the recommendations I gave her were simple exercises to reduce the sensitivity of her piriformis muscle.
But although the exercises seemed simple, I stressed to Jill that I couldn’t do the work for her. She would need to put in the time consistently to achieve results. And she did.
For the first three days, we tried two things: the McKinzie Lumbar Flexion, because during her exam it appeared that lower back arching increased her pain; and simply walking.
Visit #2 At Performance Place® Sports Care
On the fourth day, despite diligently performing these exercises, Jill returned with little-to-no change. Had I chosen her recommendations appropriately, this would be very uncommon. I typically expect a 25% to 50% improvement in piriformis cases within a week.
When Jill didn’t experience these results, I referred her to a trusted colleague. He performed an exam similar to mine. But as I suspected, he found a critical difference in one important test: her directional preference.
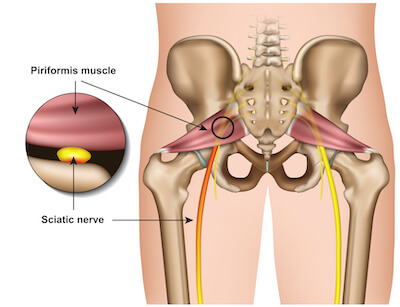
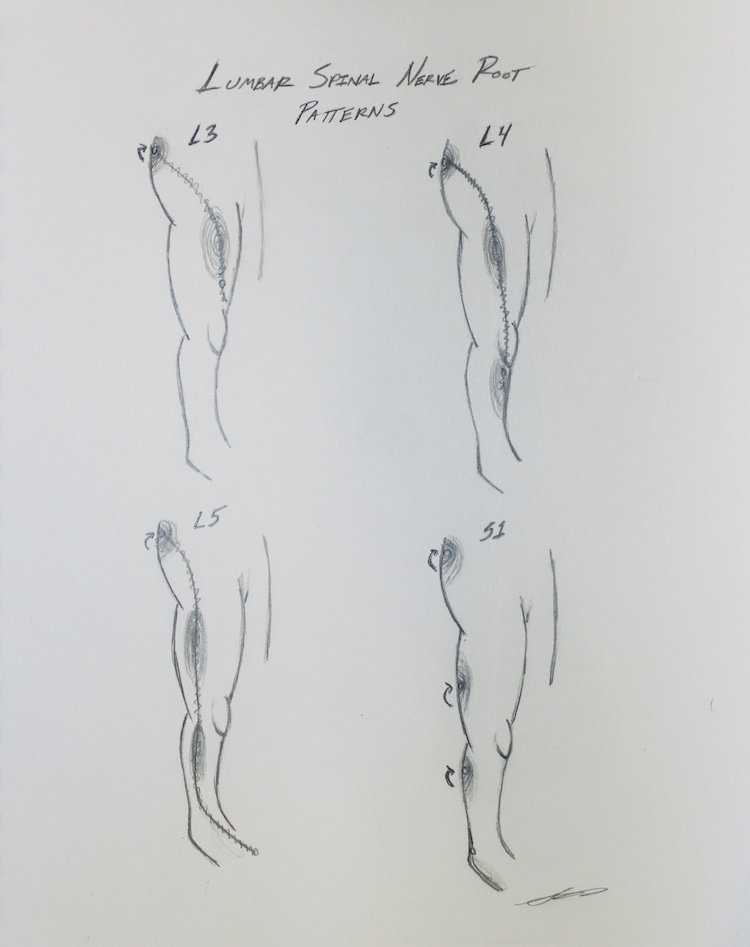
Many times, piriformis pain is being referred from a pinched nerve in the lower back. When this is the case, treatment is extremely successful if we decompress the S1 nerve root by figuring out whether bending forward or backward creates less compression. This is called directional preference.
When my colleague found Jill’s true directional preference, he was able to have her lay comfortably on the floor in a facedown book-reading position for minutes—all with zero pain! And when we used this finding to change her treatment plan, the results were even more drastic.
For the first three days, we tried two simple exercises: the McKinzie Lumbar extension, which is the opposite of low-back rounding; and walking for therapy.
After four days, Jill came in with amazing progress: a 50% reduction of symptoms! She was able to walk 100% pain-free for more than an hour, whereas before every step would create a dull ache in her piriformis muscle.
Needless to say, Jill was ecstatic. Energized by the results, she continued with “at home” exercises, where she experienced continued improvements for two weeks before we updated her plan.
Follow-Up Visit At Performance Place® Sports Care
About two weeks into her recovery, Jill and I began to focus on building her core endurance. The goal was to increase resilience in the spinal nerve, which was creating the referred tightness of her piriformis muscle. To do so, we used the following exercises:
- Birddog Exercises
- McGill Modified Curl-Up
- Side Bridge
Jill could see the light at the end of the tunnel. She was building strength in her core and was now walking pain-free up to 5 miles a day. Although she was still experiencing pain whenever she had to drive for more than 20 minutes and was walking rather than running at her Saturday workouts, we both recognized the progress we had achieved.
The last step to solidifying these improvements was to build the human engine: the hips and legs. A few of the exercises we instructed in-office were:
After two months of specific exercises, she was able to begin running again. It took her nearly six months to run at her typical pace again, but with persistence, she achieved it.
Today, that year of pain and failed treatments is firmly in the rear-view. Jill has completed her latest ironman and multiple half-marathons. And most importantly, she’s finally back to the Saturday group runs that bring her so much happiness.
Why It Worked
What did we do that was so different than all the treatments Jill had received in the past? We treated her symptoms from the root cause. In reality, 11 months of nerve pain from a lumbar disc herniation actually created Jill’s ongoing piriformis pain. Believe it or not, this happens to more people than you’d think.
Minor lumbar disc pain, for example, can create many types of pain that plague runners:
- Hip flexor tightness
- Sit bone pain
- Piriformis tightness
- Low back tightness or pain
- Tensor Fascia Lata (TFL) tightness
- Chronic IT band tension
- Calf cramping or tightness
- Knee pain with negative X-Ray & MRI
- Groin pain
- Shooting leg pain
- Deep ache in one hamstring
It’s very common for irritated discs—even without herniations—to create local chemical changes around the exiting spinal nerve root. These changes tell the hip flexor and sit bone “alarms” to sound. The piriformis pain Jill was suffering from was not the “fire.” It was the “fire alarm” located across the room from the fire.
By addressing the root cause and following a long-term recovery plan, Jill reported 50% less pain within a three-day period. And most importantly, she was back to running within a few months.
If Jill had implemented this same treatment plan in the early stages of her pain, she would have probably felt 100% within a month. All we had to do was treat her issue at the root cause!
Find Your Missing Link To Piriformis Syndrome
Today, Jill is back to her happy, active self. She doesn’t need ongoing chiropractic adjustments. She knows her body is extremely resilient and can recover from any muscle, spine, nerve or joint-related issue. All she needs is the right type of care early on.
Jill continues to refer her friends who have “tried everything” for their aches, pains and chronic tightness issues. But it’s important to remember that her experience under my care is unique. That’s because each human is unique.
There’s no cookie-cutter method of care. If someone offers a standard method of care for your problem, run away!
If you’re suffering from an issue that “no one can figure out,” please come see me for an examination because I deal with these types of cases ALL THE TIME. Most chronic issues people experience aren’t that difficult to reduce, yet they tend to give up when they’ve experienced unsuccessful treatments. (And by the way, you don’t need an MRI before you start care. Many people get better even if their MRIs say they are “broken.”)
You can get better! You are resilient! You are not broken! You are not getting “too old!”
Typically all that’s missing is a small piece of the puzzle. In Jill’s case, her missing link was treating the disc before the piriformis. Once your missing link is found, you’ll get better in leaps and bounds, just like Jill did. If you’re around the Huntington Beach area and would like to see me, use the “Book Appointment” link below.
The results are worthwhile. If you’re not in the area and cannot access a sports chiropractor near you, go to the next section of this article for our Piriformis Syndrome 4 Week Video Guide. Time and complacency are not the answer for this type of issue.
— Dr. Sebastian Gonzales DC, DACBSP®, CSCS
Preview of Piriformis 12-Week Guide
This video guide takes all the things we do in our office and neatly organizes it in the form of videos and supplementary information so you can start feeling better and running again.
Watch the preview and let us know if you have any questions.
Kayli Anderson

5 out of 5 stars!
I did first aid for two days before moving into the strength and the pain in my leg decreased over 50% in just one session of the strength work. I couldn’t believe it! I had my first pain free long run on Sunday and the pain is still gone. [Read Full Review]