Pressure in Lower Back
Are you experiencing pain and pressure in your lower back that comes in the afternoon?
Do you wake up feeling fresh in the morning, but as the day goes on, you start to feel pressure and tension build up in the center of your lower back?
In this article (updated in 2021), I will be covering diagnoses, causes, and treatment options for lower back pressure that increases as the day goes on. This article will not cover sciatica (pain past the knee), but you can read all about that in one of my other articles here.
Believe it or not, no matter how long you’ve been dealing with your low back stiffness and pressure, you can make dramatic improvements.
Not everyone will get back to feeling 100%. As a general rule, the longer you’ve had it, the more challenging it can be. But this does not mean it’s impossible to feel physically capable again.
Allow me to encourage you.
Don’t wait.
Correct it now and feel physically and mentally put back together again.
Let’s get on to the article.

Causes
- Currently Active Lumbar Disc Herniation
- Spinal Stenosis
- Osteoarthritis
- Degenerative Disc Disease
- Facet Syndrome
I’ll touch on all of these to some length.
Please do yourself a favor and read/ watch all of the resources I have provided. There are 1000 articles on lower back pressure and stiffness on the Internet, but I can assure you that there will be no need to search for more information if you read this whole article.
Currently Active Lumbar Disc Herniation
Most common cause of pressure in lower back while sitting.
Full Youtube Video Explanation
Lumbar disc herniations DO NOT require surgery, injections, or medications to treat.
They do not require X-rays or MRIs to diagnose.
You do not need to see a back surgeon before establishing a treatment plan.
These are the first questions many of our clients have.
Now that we have that out of the way. Let’s briefly discuss what active lumbar disc herniations are.
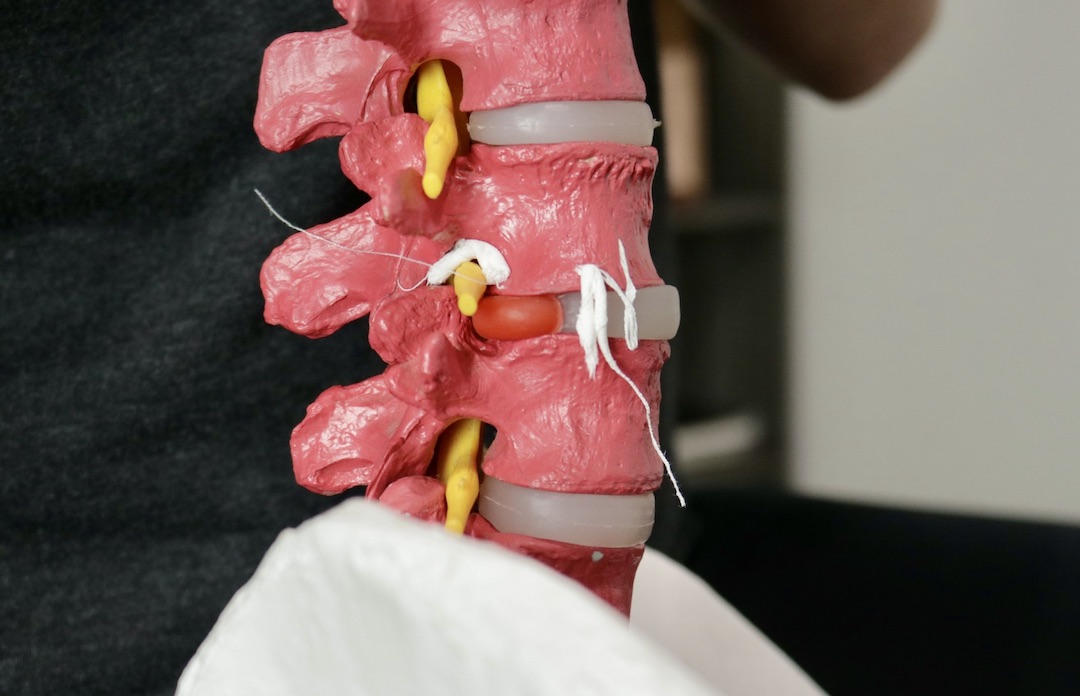
The bones of the spine are called vertebrae. The “jelly doughnuts” that space them out are called the intervertebral discs. The spinal discs are amazingly resilient. They do not blow out by stepping off curbs, bending over, or even deadlifting poorly. They can heal themselves, reabsorb, and you can feel 100% normal again if you deal with it sooner than later.
The current thought is that these discs can become “sensitive” when exposed to too much motion at a particular segment, which is possibly why you may have a normal MRI yet still have discogenic pain. MRIs are static images that do not see movement in the spine.
A trained eye is the only affordable way to see excessive spinal motion.
Excessive motion in areas like L5 and S1 occurs as the body is trying to produce a range of motion that is lacking in adjacent regions. The most common regions lacking mobility are the lower thoracic spine and the hips. While your mid-back and hips do not hurt, they do not need to lack mobility and function, contributing to daily lower back pressure.
Taking pressure off of the lumbar spine can occur with a structured program to improve mobility, stability, and strength where needed. Results can be seen in as little as a week if custom and coached 1-on-1.
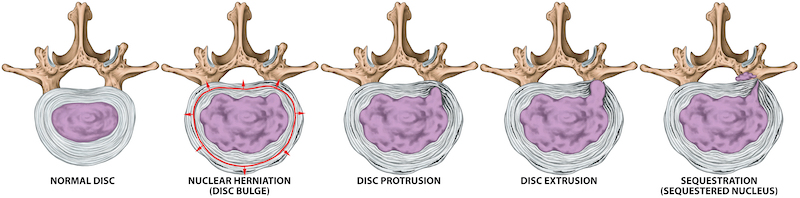
Herniations (a lower form of disc injury) are when the jelly starts to migrate to the outer section of the doughnut.
If left unaddressed (allowing excessive spinal motion), more advanced forms of non-traumatic disc injuries can occur, along with arthritis/ bone spurs. Later stages of this condition are called prolapse, extrusions, and sequestrations.
Disc prolapse and extrusions are STRONGLY related to back pain, but it would feel much more intense than just on and off lower back pressure.
I know it all sounds scary, but remember, the body is resilient, and your spinal discs will generally heal themselves with the proper steps. Papercuts heal, and so do disc injuries (trauma or not).
Most people experiencing pressure and pain in their lower back are dealing with currently active discs, which will make your lower back muscles contract to stop you from bending forward too far. This happens because the disc naturally heals itself when you limit rounding your low back for a few weeks.
Remember I said before that too much motion of the lower back could advance the condition? Your body is trying to help without you knowing it!
This protective mechanics is helpful, but it is exhausting for the muscles around your spine. It also increases compression on your spine, yielding a feeling of deep pressure. This extension stabilization strategy produces more compression on the posterior architecture of the spine, called the facet joints.
We will cover this protective mechanism in a later section.
Note: If you’re tired of reading, we have much of this information in a webinar format available on-demand for free. Take advantage here.
Spinal Stenosis
The leading cause of pressure in lower back over the age of 70.
Spinal stenosis comes in a few forms: foraminal stenosis and central stenosis. Never fear. This does not mean a death sentence for your lower back either.
Stenosis translates to “narrowing.”
When you have signs of stenosis, you have signs of holes narrowing in the spine. This typically happens as bone starts to encroach on the borders of the holes.
This usually is not inherited. It’s a sign of how your spine is adapting to the forces you placed upon it for the last 10-20 years. Above, we discussed how increased compression of the facet joints occurs as your body attempts to stabilize your lower back.
Years of spinal compression can yield more bone growth around the facet joints, which is thought to contribute to early-onset foraminal stenosis. The intervertebral foramen is the hole formed by neighboring facet joints.
More bone equals less hole space and more compression of the nerves passing through the holes, yielding sciatica.
When talking to your doctor about stenosis, don’t be afraid.
We have a saying, “Stenosis is not a problem until it is a problem.”
You have had stenosis for ten years, but your back stiffness may have just started this year. Stenosis does not happen overnight. It has severities, just like disc injuries.
The bigger question is how we can stop stenosis. My thought is to arrest the stimulus for excessive bone growth in the area with decompressive rehabilitation.
No, not that $3000 treatment plan for that big fancy table. Simple and effective exercises you should be doing daily. I shared my favorite in the sections to come.

Osteoarthritis
There are 100s of types of arthritis. The one we will be discussing is called “old age arthritis.”
Osteoarthritis is called “grey hair of the spine.”
Grey hair does not hurt, nor does osteoarthritis.
I know you may have been told differently. “Age-related back stiffness” is an old myth surrounding lower back pressure that continues to discourage people of all ages.
If I were to tell you that your back pain is because of your age, why would you not try to get better?
Exactly, we can’t beat Father Time. We have seen 100s, if not 1000s, of people who have been told their lower back pain is due to their age. They come in for their first session, saying we are the last attempt before they live with it.
Within months, most of these same people reverse their state of mind and are back to being active again!
We have seen people of all ages and severities of osteoarthritis who have fully recovered to yoga, baseball, soccer, running, and much more.
I have debunked the myth of osteoarthritis numerous times with articles cited on my website in the past.
Degenerative Disc Disease
The most overly diagnosed cause of pressure in the lower back under the age of 40.
Degeneration of the spine is another diagnosis that seems like a death sentence.
In recent years, the medical profession has started to get away from using this term as it tends to create depression and lack of motivation to improve constant low back pressure.
It sounds similar to what we discussed in the arthritis section!
Also known as DDD, degenerative disc disease is from a thinning of the intervertebral discs in the spine and the presence of bone spurs (arthritis), also known as osteophytes on X-rays.
DDD does NOT have a solid relationship to pressure, numbness, tingling, weakness, pain, tightness, or aches in your spine. Yet, some people with imaging findings of degenerative disc disease can have some of the above.
Consider this simple analogy.
When you’ve spent a weekend in the sun, you don’t always end up with a sunburn.
When you have DDD, you don’t always have pressure, numbness, tingling, weakness, pain, tightness, or aches.
Don’t worry too much if you have been given the diagnosis of degeneration of the spine. A skilled rehabilitation specialist can create simple and effective treatment plans to help with mobility, stability, and strength, yielding the results you are looking for.
We offer programs that work well in this situation. Contact us to learn more!

Facet Syndrome
Common cause of pressure in the lower back while arching your back.
Facet Syndrome is known as the inflammation, acute or chronic, of the small joints of the spine known as the facet. There are lots of these little joints in your spine, as they start at your neck and go down to your sacrum.
The old theory of why the facet joints can create pressure in the low back and neck is from a wearing away of the cartilage between the joint surfaces.
Again, this is an old theory that many outdated webpages many still promote.
The current theory is a lot more encouraging than thinking you are wearing yourself away. Now we believe you are simply placing too many stability requirements on the facet joints. You require them to do too much, and the pain you are experiencing is a plea for some better core stability, midback mobility, and hip strength.
I discussed this in the active disc section as well.
Believe it or not, simple home exercises can immediately reduce lower back pressure associated with Facet Syndrome.
Here is a powerful exercise we posted on our Youtube channel for people who place too much demand upon their facet joints.
Try the exercise at your own risk, as what you may believe to be facet pressure may not be facet pressure. If you are wrong, this exercise could increase local pain in your spine. If you’re right, it will reduce the pressure within 2 minutes.
If it does not work, remember we have 100s of exercises tailored to your situation. No workout should increase your pain or pressure. It should be effortful in the desired areas, as noted in the video.

Other Possible Diagnoses
- Sciatica (Youtube video full explanation)
- Trauma
- Compression Fracture
Non-diagnoses
The following are not diagnoses, but they can be causes for lower back pressure, pain, numbness, tingling, ache, burn, and much more. They tend to “create” the diagnoses we discussed above.
- Maladaptation/ compensation of motions
- Glute amnesia
- Tight hip flexors
- Tight hamstrings
- Tight QL muscle
- Overactive TFL muscle and IT band complex
- Lack of general physical preparedness
- Trigger points
- Muscle spasms/ Muscle strains
As I mentioned previously in the active disc section, sometimes the body is protecting against further “damage,” which results in compensations of movement.
Movement compensation can be helpful (if your disc is sensitive), or it can be a remnant from an old injury that has never been “re-programmed.”
Human movement starts with your nervous system.
The movement of muscles and joints is the result of what task your nervous system coordinated. Allow me to explain.
There are endless ways how to pick a penny off the ground. When people throw their back out, they all default to a very similar movement pattern of picking up the penny. Default patterns protect the back but also make muscle groups dormant.
Most people who throw out their lower back use their knees to accomplish the task of picking up the penny than non-injured people. Non-injured people use their hips and low back more freely.
Some of the pressure, tightness, and muscle spasms can be old guards against the old problem.
Muscles that are “turned off” need to be turned back on.
Muscles that are overactive need help. Let’s activate/ facilitate the muscles that are “turned off” to assist them.
By reducing the current problem (active disc, sciatica, facet pain, etc.), we can reprogram the muscles and movements. If the problem is no longer creating pain, we still need to reprogram, or the problem will probably return.
Reduction of pain and restoration of motion are not the same goals. They should be part of every treatment program, but they often have different timelines.
If you want to learn how to get rid of these, I’d suggest you watch the free webinar we created to help you organize your thoughts on what to do next.
The webinar includes complete explanations of the most common diagnoses, visual models, and exercises to prove to you how quickly you can feel physically capable again with our coaching.
Scary Things
We always have to include the rare but possible sinister diagnoses like a tumor, infection, cord compression, and much more.
To learn more about the “Red flags of low back pain,” go to this website this article.
Now on to more fun stuff.

Examination Of Pressure In Low Back
The best starting point is always a comprehensive examination by a low back pressure specialist. Your medical history and medical examination should take about 30 minutes. If you are in and out the door in 10 minutes, find someone who can perform a thorough test with you.
This specialist can be a sports chiropractor, sports physical therapist, physiotherapist, medical doctor, or orthopedic.
Note: Not all medical professionals have school or personal experience with this type of examination.
Don’t let a degree fool you.
Ask questions, read their website, and read online reviews of success and failure.
A simple adjustment, hot pack, injection, medication, or back surgery is NOT a comprehensive solution in most chronic lower back pressure. None of these magic tricks will turn muscles back on, make you stronger, or reprogram your movements.
If you’re within a drive of Orange County, CA, just see us. Please read our reviews. We also offer virtual sessions.

Extra Testing
Xrays, MRIs, CT scans, and Ultrasounds can be helpful but are not required in most cases of lower back pressure.
Again, you need a thorough medical examination first. Your experienced doctor can tell you if you need more advanced images or not.
Hint: We usually suggest more images when you are not responding to 6 weeks of treatment, or you have information that may lead us to believe you have one of the possible scary things creating your symptoms.
Don’t start with an MRI. It burns through the budget. Most people have to get rid of the problem, but it never tells them how to get rid of the pressure.
Broken record, I know; the comprehensive medical examination is the best start.
Non-Surgical Treatments Of Pressure In Low Back
Lower back pressure non-surgical treatments that work VERY WELL for our facility include:
- Deep tissue work (ART, Stecco, or sports massage)
- Corrective exercises
- Mobility exercises
- Stability exercises
- Strength exercises
- Modification of your daily life for a while
- Walking
These can be provided by a physical therapist, physiotherapist, occupational therapist, sports chiropractor, or even a personal trainer.
Again do not let a degree fool you. It would be best if you had someone with EXPERTISE. Check your medical provider’s reviews online.

Recap
I’m always hesitant to write articles like this because they are just a tiny peek into what is needed to overcome pressure in the lower back.
If you are suffering from chronic lower back stiffness should not be doing things on your own. Much of the reason you are in this situation is that you’ve failed to respond to past therapy (DIY or professional).
While I may sound like I’m saying people can’t overcome this on their own, I’m not.
If you’re reading this article, it’s because you cannot overcome this on your own successfully; therefore, you should hire someone to coach you through it. You would be amazed at what working with someone with experience in lower back recovery can do in just a matter of weeks.
I have had lower pain and stiffness before. I also tried to do it on my own. I failed!
I hired another good sports chiropractor who was able to tell me exactly what to do and when to do it. He coached me on HOW to do the exercises.
We have a saying, “It’s not the exercises that make you feel better. It’s HOW you do them.”
As I mentioned previously, we need to reprogram your movements. Just like a professional athlete, we all need coaches sometimes. I’m not too proud to say that I needed some professional help.
When you are ready to get rid of this ongoing problem that negatively affects your quality of life, reach out to us.
Sebastian Gonzales DC, DACBSP®, CSCS